A 60-year-old man in Germany has become at least the seventh person with HIV to be announced free of the virus after receiving a stem-cell transplant. But the man, who has been virus-free for close to six years, is only the second person to receive stem cells that are not resistant to the virus.
“I am quite surprised that it worked,” says Ravindra Gupta, a microbiologist at the University of Cambridge, UK, who led a team that treated one of the other people who is now free of HIV. “It’s a big deal.”
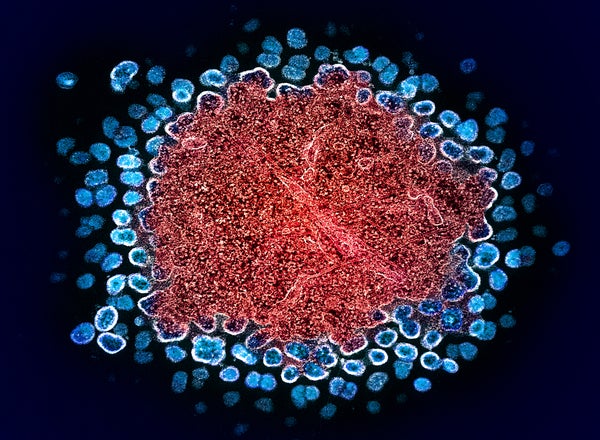
The first person found to be HIV-free after a bone-marrow transplant to treat blood cancer was Timothy Ray Brown, who is known as the Berlin patient. Brown and a handful of others received special donor stem cells. These carried a mutation in the gene that encodes a receptor called CCR5, which is used by most HIV virus strains to enter immune cells. To many scientists, these cases suggested that CCR5 was the best target for an HIV cure.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The latest case — presented at the 25th International AIDS Conference in Munich, Germany, this week — turns that on its head. The patient, referred to as the next Berlin patient, received stem cells from a donor who only had one copy of the mutated gene, which means their cells do express CCR5, but at lower levels than usual.
The case sends a clear message that finding a cure for HIV is “not all about CCR5”, says infectious-disease physician Sharon Lewin, who heads The Peter Doherty Institute for Infection and Immunity in Melbourne, Australia.
Ultimately, the findings widen the donor pool for stem-cell transplants, a risky procedure offered to people with leukaemia but unlikely to be rolled out for most individuals with HIV. Roughly 1% of people of European descent carry mutations in both copies of the CCR5 gene, but some 10% of people with such ancestry have one mutated copy.
The case “broadens the horizon of what might be possible” for treating HIV, says Sara Weibel, a physician-scientist who studies HIV at the University of California, San Diego. Some 40 million people are living with HIV globally.
Six years HIV-free
The next Berlin patient was diagnosed with HIV in 2009. He developed a type of blood and bone-marrow cancer known as acute myeloid leukaemia in 2015. His doctors could not find a matching stem-cell donor who had mutations in both copies of the CCR5 gene. But they found a female donor who had one mutated copy, similar to the patient. The next Berlin patient received the stem-cell transplant in 2015.
“The cancer treatment went very well,” says Christian Gaebler, a physician-scientist and immunologist at the Charité — Berlin University Medicine, who presented the work. Within a month, the patient’s bone-marrow stem cells had been replaced with the donor’s. The patient stopped taking antiretroviral drugs, which suppress HIV, in 2018. And now, almost six years later, researchers can’t find evidence of HIV replicating in the patient.
Shrunken reservoir
Previous attempts to transplant stem cells from donors with regular CCR5 genes have seen the virus reappear weeks to months after the people with HIV stopped taking antiretroviral therapy, in all but one person. In 2023, Asier Sáez-Cirión, an HIV researcher at the Pasteur Institute in Paris, presented data on an individual called the Geneva patient, who had been without antiretroviral therapy for 18 months. Sáez-Cirión says the person remains free of the virus, about 32 months later.
Researchers are now trying to work out why these two transplants succeeded when others have failed.
They propose several mechanisms. First, antiretroviral treatment causes the amount of virus in the body to drop considerably. And chemotherapy before the stem-cell transplant kills many of the host’s immune cells, which is where residual HIV lurks. Transplanted donor cells might then mark leftover host cells as foreign and destroy them, together with any virus residing in them. The rapid and complete replacement of the host’s bone-marrow stem cells with those of the donor’s might also contribute to the swift eradication. “If you can shrink the reservoir enough, you can cure people,” says Lewin.
The fact that both the next Berlin patient and his stem cell donor had one CCR5 gene copy with a mutation could have created an extra barrier to the virus entering cells, says Gaebler.
The case also has implications for therapies currently in early-stage clinical trials, in which the CCR5 receptor is sliced out of a person’s own cells using CRISPR–Cas9 and other gene-editing techniques, says Lewin. Even if these therapies don’t get to every single cell, they could still have an impact, she says.
This article is reproduced with permission and was first published on July 26, 2024.