Alyson Velasquez hates needles. She never liked getting shots as a kid, and her anxiety only grew as she got older. “It really ballooned in my teens and early 20s,” she says. “It became a full-blown phobia.” She would panic at the sight of a needle being brought into an exam room; more than once she passed out. Velasquez says that she took an antianxiety medication before one appointment yet still ran around the room screaming inconsolably “like I was a small child; I was 22.” After that episode Velasquez, now a 34-year-old financial planner in southern California, quit needles completely. “No vaccinations, no bloodwork. For all of my 20s it was a no-go for me,” she says.
Then COVID showed up. “It finally hit a point where it wasn’t just about me,” Velasquez says. “It felt so selfish not to do this for the greater public health and the safety of our global community.” So she got vaccinated against the SARS-CoV-2 virus in 2021, although she had to sit on her husband’s lap while he held her arms. “It was a spectacle. The poor guy at CVS ... he did ask me, ‘Are you sure you want to do this?’” She very much did. “I’m very pro-vaccine. I am a rational human. I understand the necessity of [getting] them,” she insists. But today she still struggles with each injection.
Those struggles would end, however, if all her future vaccinations could be delivered by a nasal spray. “Oh, my God, amazing!” Velasquez says.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The amazing appears to be well on its way. Vaccines delivered through the nose are now being tested for several diseases. In the U.S., early clinical trials are showing success. Two of these vaccines have generated multiple immune system responses against the COVID-causing virus in people who received them through a puff up the nose; earlier this year their makers received nearly $20 million from Project NextGen, the Biden-Harris administration’s COVID medical initiative. Researchers are optimistic that a nasal spray delivering a COVID vaccine could be ready for the U.S. as soon as 2027. Although recent efforts have focused on inoculations against SARS-CoV-2, nasal vaccines could also protect us against the flu, respiratory syncytial virus (RSV), and more.
A few nasal vaccines have been introduced in the past, but they’ve been beset by problems. The flu inoculation FluMist has not gained popularity because of debates about its effectiveness, and a different vaccine was pulled from the market decades ago because some people had serious side effects. In China and India, nasal vaccines for COVID have been approved because those countries prioritized their development during the pandemic, whereas the U.S. and other wealthy nations opted to stick with arm injections. But this new crop of vaccines takes advantage of technology that produces stronger immune responses and is safer than preparations used in the past.
In fact, immunologists say these spritzes up the nose—or inhaled puffs through the mouth—can provide faster, stronger protection against respiratory viruses than a shot in the arm. That is because the new vaccines activate a branch of the immune system that has evolved for robust, rapid responses against airborne germs. “It may be more likely to really prevent infection from getting established,” says Fiona Smaill, an infectious disease researcher at McMaster University in Ontario. Such inoculations may also help reduce the enormous inequities in vaccine access revealed by the pandemic. These formulations should be cheaper and easier to transport to poor regions than current shots.
But nasal vaccines still face technical hurdles, such as how best to deliver them into the body. And unlike injected vaccines, which scientists can measure immune responses to with blood tests alone, testing for immunity that starts in nose cells is more challenging. But researchers working in this field agree that despite the hurdles, nasal formulations are the next step in vaccine evolution.
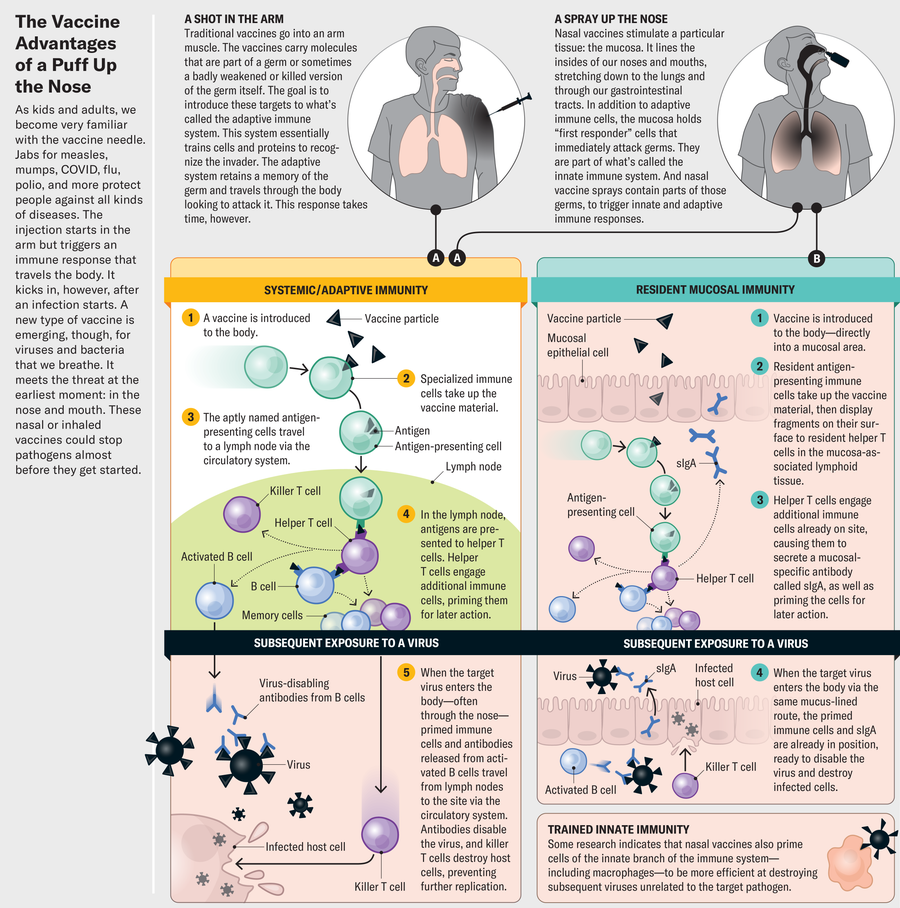
Traditional vaccines injected through the skin and into an arm muscle provide excellent protection against viruses. They coax immune cells into making widely circulated antibodies—special proteins that recognize specific structural features on viruses or other invading pathogens, glom on to them and mark them for destruction. Other immune cells retain a “memory” of that pathogen for future encounters.
Intramuscular injection vaccines are good at preventing a disease from spreading, but they do not stop the initial infection. A nasal spray does a much better job. That’s because sprays are aimed directly at the spot where many viruses first enter the body: the nose and the tissue that lines it, called the mucosa.
Mucosa makes up much of our bodies’ internal surfaces, stretching from the nose, mouth and throat down the respiratory tract to the lungs, through the gastrointestinal tract to the anus, and into the urogenital tract. Mucosa is where our bodies encounter the vast majority of pathogenic threats, Smaill says, be it flu, COVID, or bacterial infections that attack the gut. This tough, triple-layered tissue is specialized to fight off invaders with its thick coating of secretory goo—mucus—and with a cadre of resident immune cells waiting to attack. “Mucosa is really the first line of defense against any infection we’re exposed to,” Smaill says.
“We’re expecting to see fewer breakthrough infections in people who got the vaccine up the nose.”
—Michael Egan Castlevax
Mucosal immunity not only prepares the immune system for the fight where it occurs but also offers three different types of protection—at least one more than a shot does. Nasal vaccines and shots both mobilize immune messenger cells, which gather the interlopers’ proteins and display them on their surfaces. These cells head to the lymph nodes, where they show off their captured prize to B and T cells, which are members of another part of the immune system called the adaptive arm. B cells, in turn, produce antibodies, molecules that home in on the foreign proteins and flag their owners—the invading microbes—for destruction. Killer T cells directly attack infected cells, eliminating them and the microbes inside. This provides broad protection, but it takes time, during which the virus continues to replicate and spread.
That’s why a second type of protection, offered only by the mucosal tissue, is so important. The mucosa holds cells of the innate immune system, which are the body’s “first responders.” Some of these cells, called macrophages, recognize invasive microbes as foreign and swallow them up. They also trigger inflammation—an alarm sounded to recruit more immune cells.
Another part of this localized response is called tissue-resident immunity. These cells don’t have to detect telltale signs of a pathogen and make a long journey to the infected tissue. They are more like a Special Forces unit dropped behind enemy lines where a skirmish is occurring rather than waiting for the proverbial cavalry to arrive. This localized reaction can be quite potent. Its activation is notoriously difficult to demonstrate, however, so historically it’s been hard for vaccine makers to show they’ve hit the mark. But it turns out that one type of antibody, called IgA, is a good indicator of mucosal immunity because IgAs tend to predominate in the mucosa rather than other parts of the body. In an early trial of CoviLiv, a nasal COVID vaccine produced by Codagenix, about half of participants had detectable IgA responses within several weeks after receiving two doses. That trial also showed the vaccine was safe and led to NextGen funding for a larger trial of the vaccine’s efficacy.
It’s possible an inhaled vaccine may provide yet one more layer of protection, called trained innate immunity. This reaction is a bit of a mystery: although immunologists know it exists and appears also to be produced by intramuscular injections, they can’t quite explain how it works. Immune cells associated with trained innate immunity seem to have memorylike responses, reacting quickly against subsequent infections. They also have been found to respond against pathogens entirely unrelated to the intended vaccine target. Smaill and her colleagues found that when they immunized mice with an inhaled tuberculosis vaccine and then challenged them with pneumococcal bacteria, the mice were protected. In children, there is some evidence that a tuberculosis vaccine, in the arm, generates this type of broad response against other diseases.
Akiko Iwasaki, an immunologist at Yale University who is working to develop a nasal vaccination for COVID, sees two major potential benefits to nasal immunity in addition to better, faster, more localized protection. First, attacking the virus in the nose could prevent the disease from being transmitted to others by reducing the amount of virus that people breathe out. And second, Iwasaki says, the spray may limit how deeply the infection moves into the body, so “we believe that it will also prevent long COVID.” That debilitating postinfection condition, sometimes marked by signs of entrenched viral particles, disables people with extreme fatigue, chronic pain, a variety of cognitive difficulties, and other symptoms.
Making a new vaccine is hard, regardless of how you administer it. It needs to raise an immune response that’s strong enough to protect against future invasions but not so strong that the components of that response—such as inflammation and fever—harm the host.
The lining of the nose puts up its own barriers—literal, physical ones. Because the nasal mucosa is exposed to so many irritants from the air, ranging from pet hair to pollen, the nose has multiple lines of defense against invading pathogens. Nostril hair, mucus, and features called cilia that sweep the nasal surface all aim to trap small foreign objects before they can get deeper into the body—and that includes tiny droplets of vaccine.
And lots of small foreign particles—often harmless—still make it through those defenses. So the nose has developed a way to become less reactive to harmless objects. This dampened reactivity is called immunological tolerance, and it may be the biggest hurdle to successful development of a nasal vaccine. When foreign particles show up in the bloodstream, a space that is ostensibly sterile, immune cells immediately recognize them as invaders. But mucosal surfaces are constantly bombarded by both pathogens and harmless materials. The immune system uses tolerance—a complex series of decisions carried out by specialized cells—to determine whether a substance is harmful. “This is very important because we can’t have our lungs or gastrointestinal tract always responding to nonharmful foreign entities that they encounter,” says Yale infectious disease researcher Benjamin Goldman-Israelow. For example, inflammation in the lungs would make it hard to breathe; in the gut, it would prevent the absorption of water and nutrients.
Jen Christiansen; Source: Florian Krammer, Icahn School of Medicine at Mount Sinai and Medical University of Vienna, Austria (consultant)
These barriers may hamper the effectiveness of a nasal flu vaccine that’s been around for a while, called FluMist in the U.S. and Fluenz in Europe. The inoculation is safe, says infectious disease scientist Michael Diamond of Washington University in St. Louis, but it faces a similar problem as do injected flu vaccines: it isn’t very effective at warding off new seasonal flu strains. This might be because flu strains are so common, and people are frequently infected by the time they are adults. Their immune systems are already primed to recognize and destroy familiar flu particles. FluMist is built from a live flu virus, so immune cells probably treat the vaccine as an invader and demolish it as soon as it shows up in the nose, before it has a chance to do any good. This preexisting immunity isn’t such an issue in children, who are less likely to have had multiple flu infections. Nasal flu vaccines are routinely used to inoculate kids in Europe.
In other vaccines, researchers often use adjuvants, special agents that attract the attention of immune cells, to boost a response. Some nasal vaccines use adjuvants to overcome tolerance, but in the nose, adjuvants can pose unique dangers. In at least one case, a nasal adjuvant led to disastrous consequences. An intranasal vaccine for influenza, licensed in Switzerland for the 2000–2001 season, used a toxin isolated from Escherichia coli bacteria as an adjuvant to provoke a reaction to the inactivated virus. No serious side effects were reported during the trial period, but once the vaccine was released, Swiss officials saw a concerning uptick in cases of Bell’s palsy, a disease that causes weakness or paralysis of the facial muscles, often leading to a drooping or disfigured face. Researchers at the University of Zurich estimated that the adjuvanted flu vaccine had increased the risk of contracting Bell’s palsy by about 20 times, and the vaccine was discontinued. “We need to be cautious about using adjuvants like that from known pathogens,” says pharmaceutical formulations scientist Vicky Kett of Queen’s University Belfast in Northern Ireland.
To get around the challenges posed by the nose, some researchers are exploring vaccines inhaled through the mouth. Smaill is working on one of them. She and her McMaster colleagues aerosolized their vaccine for COVID into a fine mist delivered by a nebulizer, from which it rapidly reaches the lungs. Experiments in mice have shown promising results, with mucosal immunity established after administration of the vaccine.
Another vaccine strategy is to use a harmless virus to carry viral genes or proteins. Researchers at the Icahn School of Medicine at Mount Sinai in New York City selected a bird pathogen, Newcastle disease virus (NDV). “It’s naturally a respiratory pathogen,” so it infects nasal cells, says Michael Egan, CEO and chief scientific officer of CastleVax, a company that formed to develop the NDV vaccine for COVID. A small early clinical trial showed the CastleVax vaccine was safe and caused robust immune responses in people. “Those results were very promising,” Egan says. People who received the vaccine also produced antibodies that indicated multitiered mucosal immunity, not simply the adaptive immunity from a shot in the arm.
Following that trial, the CastleVax project received NextGen funding, and results from a trial of 10,000 people are expected in 2026. Half of those people will receive a messenger RNA (mRNA) injection, and half will get the new NDV nasal spray. The data should show whether the new nasal vaccine can do a better job of preventing infection than the mRNA injections. Egan has high hopes. “We’re expecting to see a lot fewer breakthrough infections in people who got the vaccine up the nose by virtue of having those mucosal immune responses,” he says.
Florian Krammer, one of the Mount Sinai researchers behind the vaccine, engineered NDV particles to display a stabilized version of the spike protein that’s so prominent in SARS-CoV-2. “You end up with a particle that’s covered with spike,” he says. Spike protein in the bloodstream can raise an immune response. But the NDV vaccine works in another way, too. The virus particle can also get into cells, where it can replicate enough times to cause virus particles to emerge from the cells, provoking another immune reaction. Before moving into human trials, however, researchers had to complete clinical trials to establish that the Newcastle virus is truly harmless because the nose is close to the central nervous system—it has neurons that connect to the olfactory bulb, which is part of the brain. Those trials confirmed that it is safe for this use.
Nasal sprays aim directly at the spot where most viruses first enter the body: the nose.
This type of caution is one reason a COVID nasal vaccine approved in India hasn’t been adopted by the U.S. or other countries. The inoculation, called iNCOVACC, uses a harmless simian adenovirus to carry the spike protein into the airway. The research originated in the laboratories of Diamond and some of his colleagues at Washington University at the start of the pandemic, when they tested the formulation on rodents and nonhuman primates. “The preclinical data were outstanding,” Diamond says. Around the time he and his colleagues published initial animal results in Cell in 2020, Bharat Biotech in India licensed the idea from the university. In a 2023 phase 3 clinical trial in India, the nasal vaccine produced superior systemic immunity compared with a shot.
Diamond says American drug companies didn’t pursue this approach, because “they wanted to use known quantities,” such as the mRNA vaccines, which were already proving themselves in clinical trials in 2020. As the pandemic took hold, there was little appetite to develop nasal vaccine technology to stimulate mucosal immunity while the tried-and-true route of shots in the arm was available and working. But now, four years later, an inhaled vaccine using technology similar to iNCOVACC’s is being developed for approval in the U.S. by biotech company Ocugen. Both inhaled and nasal forms of the vaccine are set to undergo clinical trials as part of Project NextGen. These new vaccines are using classical vaccine methods based on the virus rather than using new, mRNA-based technology. The mRNA preparations were developed specifically for intramuscular injections and would have to be significantly modified.
Codagenix, which is developing CoviLiv, sidestepped the need for a new viral vector or an adjuvant by disabling a live SARS-CoV-2 virus. To make it safe, scientists engineered a version of the virus with 283 mutations, alterations to its genetic code that make it hard for the virus to replicate and harm the body. Without all these genetic changes, there would be a chance the virus could revert to a dangerous, pathogenic form. But with hundreds of key mutations, “statistically, it’s basically impossible that this will revert back to a live virus in the population,” says Johanna Kaufmann, who helped to develop the vaccine before leaving Codagenix for another company earlier this year.
Because most people on the planet have now been exposed to SARS-CoV-2—in the same way they’re regularly exposed to the flu—some nasal vaccines are being designed as boosters for a preexisting immune response that is starting to wane. For example, Yale researchers Iwasaki and Goldman-Israelow are pursuing a strategy in animals deemed “prime and spike.”
The idea is to start with a vaccine injection—the “prime” that stimulates adaptive immunity—then follow it a few weeks later with a nasal puff that “spikes” the system with more viral protein, leading to mucosal immunity. In a study published in 2022 in Science, Iwasaki and her colleagues reported that they primed rodents with the mRNA vaccine developed by Pfizer and BioNTech, the same shot so many of us have received. Two weeks later some of the mice received an intranasal puff of saline containing a fragment of the SARS-CoV-2 spike protein. Because the animals had some preexisting immunity from the shot, the researchers didn’t add any adjuvants to heighten the effects of the nasal puff. Two weeks later researchers detected stronger signs of mucosal immunity in mice that had received this treatment compared with mice that got only the shot.
“Not only can we establish tissue-resident memory T cells” to fight off the virus in the nose, Iwasaki says, but the prime-and-spike method also produces those vigorous IgA antibodies in the mucosal layer. “And that’s much more advantageous because we can prevent the virus from ever infecting the host,” she notes. The study suggests that this approach might also lessen the chances of transmitting the disease to others because of the lower overall viral load. Experiments in hamsters demonstrated that vaccinated animals shed less virus, and they were less likely to contract COVID from infected cage mates that had not been vaccinated themselves.
Although most of the new vaccine strategies are aimed at COVID, nasal vaccines for other diseases are already being planned. Kaufmann, formerly of Codagenix, says the company currently has clinical trials underway for nasal vaccines against flu and RSV. CastleVax’s Egan says “we have plans to address other pathogens” such as RSV and human metapneumovirus, another leading cause of respiratory disease in kids.
Vaccines that don’t need to be injected could clear many barriers to vaccine access worldwide. “We saw with COVID there was no vaccine equity,” Smaill says. Many people in low-income countries never received a shot; they are still going without one four years after the vaccines debuted.
In part, this inequity is a consequence of the high cost of delivering a vaccine that needs to stay frozen on a long journey from manufacturing facilities in wealthy countries. Some of the nasal sprays in development don’t need deep-cold storage, so they might be easier to store and transport. And a nasal spray or an inhaled puff would be much easier to administer than a shot. No health professional is required, so people could spray it into their noses or mouths at home.
For these reasons, needle-free delivery matters to the World Health Organization. The WHO is using the Codagenix nasal spray in its Solidarity Trial Vaccines program to improve vaccine equity. The CoviLiv spray is now in phase 3 clinical trials around the world as part of this effort. “The fact that the WHO was still interested in a primary vaccination trial in the geographies it’s passionate about—that’s indicative that there is still a gap,” Kaufmann says. CoviLiv was co-developed with the Serum Institute of India, the world’s largest maker of vaccines by dose. The partnership enabled production at the high volume required for Solidarity.
The CastleVax vaccine with the NDV vector provides another layer of equity because the facilities required to make it already exist in many low- and middle-income countries. “The cool thing is that NDV is a chicken virus, so it grows very well in embryonated eggs—that’s exactly the system used for making flu vaccines,” Krammer says. For example, for a clinical trial in Thailand, “we just shipped them the seed virus, and then they produced the vaccine and ran the clinical trials,” he says. Many countries around the world have similar facilities, so they will not need to depend on pharma companies based in richer places.
Even high-income countries face barriers to vaccination, although they may be more personal than systemic. For very many people, the needle itself is the problem. Extreme phobia such as Velasquez’s is uncommon, but many people have a general fear of needles that makes vaccinations stressful or even impossible for them. For about one in 10 people needle-related fear or pain is a barrier to vaccinations, says C. Meghan McMurtry, a psychologist at the University of Guelph in Ontario. Needle fear “is present in most young kids and in about half of adolescents. And 20 to 30 percent of adults have some level of fear.” A review of studies of children showed that “concern around pain and needle fear are barriers to vaccination in about 8 percent of the general population and about 18 percent in the vaccine-hesitant population,” McMurtry adds.
Some people are wary of injected vaccines even if they’re not afraid of needles, Kett says; they see injections as too invasive even if the needle doesn’t bother them. “We’re hopeful that something administered by the nasal route would be less likely to come across some of those issues,” Kett says.
In the U.S., however, sprays and puffs won’t be available until they are approved by the Food and Drug Administration, which requires clear evidence of disease protection. As Diamond points out, standards for such evidence are well established for injections, and vaccine makers can follow the rule book: regulations point to particular antibodies and specific ways to measure them with a simple blood test. But for nasal vaccines, Iwasaki says, “we don’t have a standard way to collect nasal mucus or measure antibody titers. All these practical issues have not been worked out.”
Iwasaki is also frustrated with a restriction by the U.S. Centers for Disease Control and Prevention that stops researchers from using existing COVID vaccines in basic research to develop new nasal sprays. The rule is a holdover from 2020, when COVID injections had just been developed and were in short supply; people had to wait to get vaccinated until they were eligible based on factors such as age and preexisting conditions. “That made sense back then, but those concerns are years old; things are different now,” Iwasaki says. “Now we have excess vaccine being thrown out, and we cannot even get access to the waste, the expired vaccine.”
Today scientists want to contrast the effectiveness of nasal formulations with injections already in use. “Those comparisons are really important for convincing the FDA that this is a worthy vaccine to pursue,” Iwasaki says. But the restriction has held up studies by her company, Xanadu, slowing down work. (The CDC did not respond to a request for comment.)
Despite the bureaucratic and scientific hurdles, the sheer number of nasal vaccines now in clinical trials encourages Iwasaki and other scientists pursuing the needle-free route. They say it seems like only a matter of time before getting vaccinated will be as simple as a spritz up the nose.
Velasquez, for one, can’t wait for that day to arrive. The circumstances that finally forced her to reckon with her fear of needles (a global pandemic, the prospect of parenthood and the numerous blood tests that accompanied her pregnancy) were so much bigger than her. If not for them, she might still be avoiding shots. “So having vaccines without needles—I would get every vaccine any doctor wanted me to get, ever. It would be a complete game changer for me.”

