On Wednesday the director general of the World Health Organization declared the mpox outbreak in the Democratic Republic of the Congo (DRC) and a few other African nations a public health emergency of international concern (PHEIC). A PHEIC is the highest level of alarm that can be issued by the WHO. Director General Tedros Adhanom Ghebreyesus described the rapid spread of a new viral group, or clade, of mpox in the eastern DRC and the reporting of cases in several neighbouring countries as “very worrying.” The situation necessitates a coordinated international response to “stop these outbreaks and save lives,” he said. Sweden has also confirmed its first case of the new clade, suggesting the spread of this form of mpox may be broader than reported.
More than 15,600 cases and 537 deaths have been reported in the current outbreak, with the DRC accounting for about 96 percent of the cases. Twelve other African countries have also reported cases—some for the first time.
A PHEIC is declared in response to an extraordinary event that poses a public health risk through the international spread of disease and requires a coordinated international response. This is not the first time a PHEIC has been declared for mpox—the WHO made a similar declaration in 2022 during a rapidly spreading multicountry mpox outbreak in which the disease was primarily sexually transmitted (though the mpox virus can also spread through close contact of any kind). The PHEIC ended in May 2023, following a sustained decline in global cases.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The populations affected by the current mpox outbreak are broader than those who were affected in the one that occurred in 2022. They range from sex workers and children in the DRC to people living with HIV in South Africa. The WHO is advocating for improved and standardized testing and surveillance.
About 24 hours before the WHO’s declaration, the Africa Centers for Disease Control and Prevention (Africa CDC) issued its first-ever declaration of a Public Health Emergency of Continental Security for mpox. At a press conference, Africa CDC’s director general Jean Kaseya said that the emergence and rapid spread of mpox is “a menace that knows no boundaries, no race, no creed.”
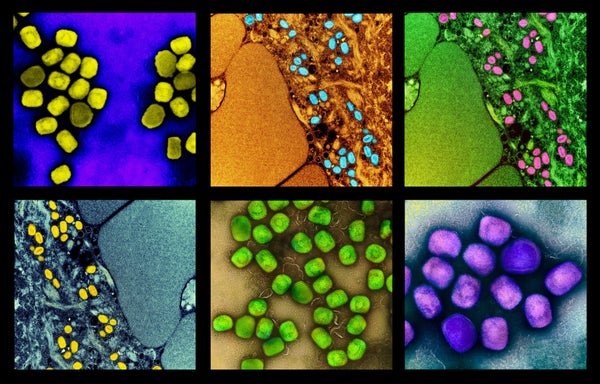
Mpox is a viral disease that typically begins with a fever, intense headache, swollen lymph nodes and muscle aches, followed by a characteristic rash that progresses through different stages. Often painful, the rash eventually forms scabs or crusts and can last for two to four weeks.
The WHO is considering two vaccines for emergency use. The DRC and Nigeria had already issued regulatory approvals for the vaccines in those countries. Kaseya estimated Africa’s need for mpox vaccines at 10 million doses but revealed that only 200,000 are available. The nonprofit Gavi, the Vaccine Alliance, said in a statement that it has accelerated engagement with manufacturers, including Bavarian Nordic, about potential direct procurement of mpox vaccines to support the outbreak response. Gavi also plans to establish a stockpile of mpox vaccines.
Experts have expressed concerns that a lot more could have been achieved earlier. Aggrey Aluso, director for the Africa region at the Pandemic Action Network, saysthat the mpox response on the continent has been slow. At the end of June, while the monthly change in confirmed cases of mpox dropped in all other regions, cases increased by 20 percent in African countries. And this trend in Africa was driven mainly by a rise in the number of cases in the DRC.
“Despite early signs of the mpox outbreak, the response has been slow and underresourced, particularly in regions, like the DRC, where the virus has had fatal consequences,” Aluso says.
Scientific American spoke with Aluso about the mpox emergency and the response so far.
[An edited transcript of the interview follows.]
How would you describe the level of preparedness for this emergency?
We lack the necessary tools and capacities, such as diagnostics, laboratory supplies and stockpiles of vaccines and treatments to quickly detect, track and contain the mpox outbreak. We don’t have diagnostics. Our laboratory systems are not up to speed across the board to really track the pathogens that are being monitored in real time. So it takes a long time to even ascertain what we’re dealing with within many jurisdictions.
It’s taking [authorities] inordinately long to even ascertain that [a given] country has reported one case. By the time they’re doing that, probably, it’s taken 10 or 20 days to go through the processes of taking samples from one region to another to do genomic sequencing, to know what they are dealing with.
We don’t have all the tools. What we’ve heard most recently is that some 50,000 doses of vaccines were available to the DRC—50,000 against the population of more than 99 million people. We should have moved much faster when this current outbreak [ramped up] in May.
Given the declaration of the mpox outbreak as a public health emergency of international concern, what steps should be taken next?
Declaring the mpox outbreak a public health emergency is necessary, but it should have been done sooner. Moving forward, there needs to be a rapid mobilization of resources, including diagnostics, vaccines and trained health workers. The global community must also act in solidarity, recognizing that an outbreak in Africa can quickly become a global issue. Africa’s leaders must take charge, ensuring that resources are allocated and used effectively to contain the outbreak before it spreads further.
How do other health priorities in Africa affect the response to health emergencies such as the mpox outbreak?
Issues such as malnutrition in children and the high prevalence of HIV exacerbate the impact of new health challenges. In regions like the DRC, children are disproportionately affected by mpox because of underlying vulnerabilities. Similarly, in South Africa, key populations such as men who have sex with men are at higher risk as a result of the intersection of mpox and the HIV epidemic. Addressing these overlapping challenges requires a more integrated and resilient health system that can support marginalized populations while responding to emerging threats.
How does Africa’s current response to the mpox outbreak compare with its response to the COVID pandemic?
Africa’s response to the COVID pandemic raised hopes that the continent would prioritize health security moving forward. The response to the mpox outbreak reveals significant gaps, however. Although there were ambitions such as Africa’s new public health order and the plan to increase vaccine manufacturing capacity, these haven’t translated into effective action.
Despite increasing disease outbreaks, Africa’s response capacity remains limited, which is concerning. The current mpox outbreak, which has spread rapidly across the continent, underscores this vulnerability.
Why do African countries still struggle to make health a budgeting priority despite previous commitments such as the Abuja Declaration, in which governments on the continent agreed to spend a minimum of 15 percent of their annual budget on health, and the lessons learned from COVID?
The challenge lies in translating lofty declarations into actionable investments. Governments often make commitments without allocating the necessary resources to fulfill them. It’s crucial for citizens to hold their governments accountable and demand that health be prioritized in national budgets. This is essential not only for responding to current outbreaks but also for building long-term resilience against future health threats.
What thoughts do you have on Africa’s public health challenges and the way forward?
Africa’s public health challenges are significant, but they are not insurmountable. We need a more coordinated and well-resourced response to health emergencies, driven by both local leadership and global solidarity. Strengthening health systems, enhancing local capacities and ensuring that resources are available when and where they are needed will be key to preventing future outbreaks from spiraling out of control. The time to act is now, and it requires a collective effort from all stakeholders.