This article is part of “Innovations In: Sickle Cell Disease,” an editorially independent special report that was produced with financial support from Vertex Pharmaceuticals.
Kalpna Gupta was in a convention center banquet hall when a child changed the course of her career. As she recalls it, she had come to Ohio around 2008 for a conference on sickle cell disease because her laboratory was studying the misshapen red blood cells that define the ailment. Typically such conferences consist of one lecture after another, each full of slides on molecular mechanisms and chemical pathways, interspersed with talks from patient advocates and caregivers.
This time a 10-year-old boy described the bouts of debilitating pain he experienced as a result of his illness. Deeply moved by his words, Gupta imagined what it would be like if her own daughter were the one suffering. She turned to colleagues sitting next to her and asked, “Who works on pain in sickle cell disease?”
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
The answer at the time was hardly anyone. Gupta remembers only one presentation on pain at the meeting, a poster by Wally R. Smith of Virginia Commonwealth University. This work was the field’s first attempt to assess the extent of discomfort associated with the disease. Smith and his team discovered that sickle cell pain was more frequent and severe than researchers or physicians realized. In addition to the acute, excruciating attacks that are characteristic of the disease, they found that nearly a third of their study participants experienced chronic, sometimes daily pain, often in their back or joints.
It was a watershed result both for the field and for Gupta, who returned to her lab at the University of Minnesota and launched her own research program on sickle cell pain. In the 16 or so years since then, Gupta—who is now at the University of California, Irvine—has started, along with Smith and other researchers, to illuminate the complex processes involved in acute and chronic pain. This work has transformed the way scientists are understanding and developing treatments for sickle cell disease.
New medications target the underlying mechanisms of sickle cell [see “New Treatments for Sickle Cell Disease,” by Sara Reardon], sometimes reducing the frequency of acute attacks, but none is designed specifically to relieve pain once it starts. There is an urgent need to better address the illness’s most prominent symptom: pain so agonizing it can harm people’s careers, relationships and lives.
In the U.S., sickle cell disease is usually diagnosed through newborn screenings done shortly after birth. Screening is more inconsistent in other countries, particularly those in sub-Saharan Africa, where the disease is most common [see “Investing in Sickle Cell Disease,” by Ambroise Wonkam]. Early symptoms, which can include painful swelling in the hands and feet, generally begin when the patient is between six and nine months old, says Deepika Darbari, a hematologist at Children’s National Hospital in Washington, D.C. As kids get older, they are struck with acute bouts of pain that last up to a week or more. These attacks happen an average of three times a year and account for 95 percent of hospital visits related to sickle cell disease. Known as vaso-occlusive crises (VOCs) or simply “crises,” these events may be associated with the development of complications—such as liver and kidney issues, strokes, a pneumonialike lung disease called acute chest syndrome, and multiorgan failure—that can result in death.
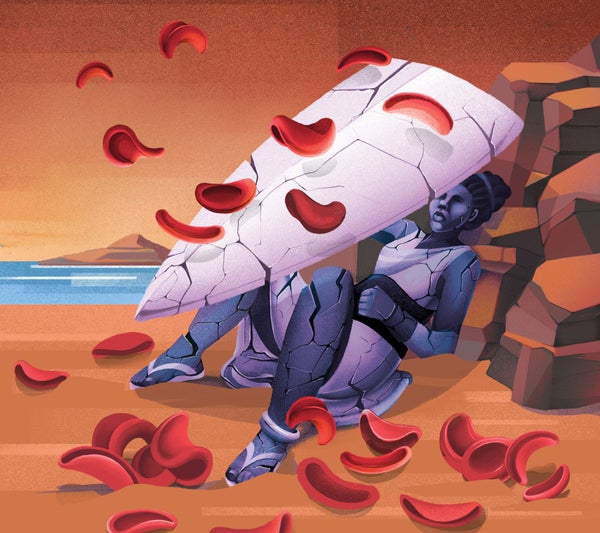
Researchers have been stymied in their attempts to ease these patients’ agony. In 1956 a University of Tennessee physician wrote, “The severe pain causes patients to grunt, groan, cry, twist and turn and to assume abnormal postures in the futile attempt to obtain relief.” The pain most often occurs in the lower back, joints, arms, legs and core, and patients describe it in almost every possible form: sudden, throbbing, sharp, but also steady and gnawing like a toothache. In a Reddit forum dedicated to the disease, people compared the sensations to being stabbed repeatedly from the inside, to hitting a bruise with a needle-covered hammer, and to a knife being dug into them and then moved around. When asked to rate their pain on a scale from 1 to 10, Darbari says, people often say they can’t give a number because it is too unyielding, but they rank it as worse than childbirth or postoperative pain. Sickle cell pain, Gupta says, “is thought to be the worst thing known to humankind.”
Nearly a century passed between the first descriptions of the disease in Western medical literature and Smith’s study, which refuted the long-held assumption that patients existed in one of only two states: pain-free or suffering from intermittent events. Instead the research—which relied on six months of daily diary entries from 232 people ages 16 and up—showed that 29 percent of study subjects had chronic pain more than 95 percent of the time, whereas just 14 percent experienced it rarely.
Additionally, although the reported pain intensity was higher than researchers had previously thought, Smith and his colleagues found that people typically went to the hospital only when they were in the middle of an acute attack. Overall, participants reported pain on 56 percent of the study days and acute crises on 13 percent but sought care on just 4 percent of them. The data made it crystal clear: physicians understood the disease based solely on what they saw in clinic, which had led them to vastly underestimate their patients’ suffering. The researchers concluded that undertreatment was common, noting that “pain in adults with sickle cell disease is the rule rather than the exception.”
These findings shifted the thinking about sickle cell. It is now recognized as a chronic disease in which repeated acute pain events transform the nervous system in ways that echo other conditions such as fibromyalgia, irritable bowel syndrome and phantom limb pain. “We havereconceptualized pain in sickle cell disease completely as a result,” Smith says. “Sickle cell disease is a window into studying all chronic pain.”
For decades experts assumed that because the misshapen red blood cells of sickle cell patients get stuck in blood vessels, blocked blood flow was causing pain wherever obstructions occurred. “In the past we thought it was a very simple thing—like, you have the vaso-occlusion, the person gets pain,” Darbari says. “The vaso-occlusion gets resolved, and the pain goes away.”
Growing evidence, however, suggests that pain sources are various and complex, leading some experts to push for a new description of attacks such as “acute pain events” or “acute pain episodes,” says Amanda Brandow, a pediatric hematologist at the Medical College of Wisconsin in Milwaukee. Although many still call them “crises,” such a linguistic shift reflects the idea that pain results from multiple causes, not just vaso-occlusion.
The nociceptive system, which registers pain, is one player. It’s triggered by multiple processes in sickle cell disease, including aggregations of various cells—sickled red blood cells, white blood cells, platelets, and other types—that adhere to the lining of blood vessels. The clumped cells block blood flow, deprive tissues of oxygen and damage the vessel lining while activating inflammation-related cells such as platelets, macrophages and mast cells, as well as molecules such as cytokines.
“There’s a tremendous pall of suspicion that circles around sickle cell disease.”
—C. Patrick Carroll Johns Hopkins University School of Medicine’s Sickle Cell Center for Adults
Gupta has found in mouse models of sickle cell disease that acute attacks injure peripheral nerves and vessels in the skin, changing the signal transmission in the spinal cord in a vicious cycle that amplifies pain. These mice show hypersensitivity to cold, heat and even small amounts of pressure, mimicking the experience of people with the disease, who may find even a strong gust of wind unbearable.
Inflammation gets worse with each acute episode, according to studies done mostly in mice, leading to more serious complications. Eventually the cycle can alter the spinal cord and brain in ways that continue to amplify pain from the lightest touch. That can happen even when there is no ongoing vaso-occlusion, says Darbari, who studies brain-activation patterns to better understand this sensitization process. According to C. Patrick Carroll, director of psychiatric services at the Johns Hopkins University School of Medicine’s Sickle Cell Center for Adults, sickle cell seems to change the nervous system in ways “that can amplify, facilitate, maybe even generate pain perception.”
Four disease-modifying medications have been approved by the U.S. Food and Drug Administration for sickle cell, and some have shown modest benefit in preventing painful events. But they can’t alleviate pain once it starts.
So far attempts to treat acute pain with pharmaceuticals have mostly fizzled. For example, in a placebo-controlled, randomized trial of l-glutamine, which can reduce adhesion, those in the test group experienced three painful events, compared with four in the placebo group. The pain of those acute attacks, however, was no less intense in the test group. “Trying to moderate the actual pain is something that I think we still need to do,” Brandow says. “We need to target the pain source.”
For now people typically have a home protocol they start at the onset of an acute event. It usually includes opioids (such as oxycodone), heat, and ibuprofen or other over-the-counter pain relievers, Darbari says. If those approaches fail, more intensive hospital care can include intravenous opioids and fluids, ketamine and local anesthesia, among other strategies. Yet even with those efforts, patients often remain in pain after discharge.
Opioids raise other concerns, too. Studies show that they might make things worse physiologically by increasing certain types of inflammation, including through the activation of immune cells called mast cells. Plus, sickle cell patients often require large opioid doses at regular intervals, which can leave them open to suspicion and accusations of drug seeking. With sickle cell in particular, Carroll says, providers accuse patients of faking or magnifying their pain to get drugs. “There’s just a tremendous pall of suspicion that circles around sickle cell disease,” he says.
The problem runs deep. “The pain that people have at home every day, silently, is slowly rotting their whole psychosocial milieu and causing stigma because nobody can see it. So they get accused of faking,” Smith says.
Given opioids’ reputation for causing addiction and overdose deaths, Darbari notes, families sometimes refuse the drugs even when their children are sobbing in pain. Whether sickle cell patients are more or less prone to addiction remains an unstudied question, Gupta says.
A number of medications for targeted, effective relief are now in various stages of investigation, including a drug known as rivipansel. This medication targets an adhesion molecule called E-selectin with the goal of preventing leukocytes from sticking to blood vessels. In a phase 3 trial, those who took rivipansel showed a 61 percent reduction of E-selectin levels in their blood. Patients who took the drug within 26 hours of an acute attack’s onset had shorter hospital stays and spent half as long on IV opioids compared with those who took it after that window—two days instead of four. But because most study participants weren’t dosed that early, the research team concluded that future trials must better assess treatment timing.
Another contender is imatinib, a cancer drug that appears to reduce inflammation. It inhibits a neuropeptide called substance P, which activates mast cells, causing inflammation and pain. Imatinib reduces VOC pain in mouse models of sickle cell disease and has shown potential to do the same in people. Studies show that adding imatinib to outpatients’ treatment protocol reduced the number of VOCs and hospitalizations and shortened hospital stays. The drug also reduced the use of pain relievers significantly.
Given that so many pathways appear to lead to acute sickle cell pain, scientists are casting a wide net. “There are a lot of drugs in the pipeline,” Brandow says.
Chronic pain in sickle cell patients generally emerges in adolescence or early adulthood. It affects up to half of all adults with the disease and can last for months, becoming a part of daily life and manifesting in various ways: joint stiffness, bone pain, nerve pain, and more. Acute pain and chronic pain seem to involve different pathways; one clue, Brandow says, is that people whose sickle cell disease is cured by bone marrow transplants often continue to experience daily discomfort. It is too soon to know whether newly approved gene therapies will relieve chronic pain, she adds, because clinical trials didn’t address that question.
Given the differences, researchers are investigating approaches that address both underlying mechanisms of chronic pain and patients’ perception of that pain. On the pharmaceutical side, Gupta’s work in mice suggests that cannabinoids may alleviate chronic pain by reducing inflammation and interrupting key pathways. There is also some promising evidence in results from studies on other debilitating pain conditions. In people with multiple sclerosis, for example, an oral cannabis spray called Sativex helps to alleviate neuropathic pain and muscle spasticity, both of which are also common symptoms of chronic sickle cell disease. Studies show that cannabinoids can act synergistically to improve the pain-relieving effects of opioids. And they ease ischemia-reperfusion injury, damage that occurs when blood flow is restored after a blockage, which can happen during or after a stroke but also is common in people with sickle cell disease. Anecdotally, many sickle cell patients report self-treating with—and achieving relief from—cannabinoid drugs. Gupta notes that research on these compounds specifically with sickle cell patients is needed but has been difficult to fund.
The microbiome is another intriguing target, Brandow says. She is wrapping up a large study, funded by the National Institutes of Health and the National Heart, Lung, and Blood Institute, assessing the differences in intestinal microbes between people with and without sickle cell. The project is also evaluating whether microbial communities change during acute events because prior studies suggested that certain gut microbes can upregulate specific immune pathways. And Brandow is investigating whether altering the microbiome to interfere with this process could reduce pain—something that has worked in sickle cell mice dosed with probiotics.
Another important approach, Smith says, will be interrupting pain signals in the nervous system. He believes it is particularly important to focus on children and adolescents before their brains develop a “nociplastic pain pattern,” pain sensitivity that sets in after years of repetitive acute attacks. That won’t necessarily require new drugs. Rather Smith suspects that doctors could prevent chronic pain, or at least diminish it, by providing better treatment to patients at younger ages.
Other factors that exacerbate chronic pain are loneliness, depression, malnutrition and social isolation, all common issues for people with sickle cell disease. Depression in particular affects between 20 and 60 percent of people with sickle cell, and studies suggest that treatment with antidepressants may reduce pain episodes. Companionship and a healthy diet might help, and those changes may also decrease the dose of opioids required to relieve pain, according to a mouse study by Gupta.
Treating both acute and chronic pain will ultimately require addressing health-care disparities, Carroll says. In a study of 291 people with sickle cell disease, most of whom were Black, Carroll, Carlton Haywood, Jr., of the Johns Hopkins School of Medicine and their collaborators found that discrimination by health-care providers resulted in increased reports of chronic pain and higher pain severity. That study was published in 2014, but research continues to reveal high rates of stigma, racial bias and discrimination affecting this patient population, all of which can exacerbate pain. Haywood died of complications from sickle cell in 2021.
The best treatment will vary by individual, says Darbari, who advocates for a “whole-person approach.” In her clinic, she aims to help children and families learn how to cope with the disease and manage their pain. Depending on a person’s situation, they might benefit from a combination of medications; lifestyle changes that could include mindfulness exercises, massage, physical activity or stretching; and psychological interventions such as cognitive-behavioral therapy to address anxiety and catastrophizing, which can make pain worse.
In a trial published this year, adolescents with sickle cell disease who completed a 12-week, app-based program that taught them techniques for relaxation, goal setting and building a social community reported fewer pain days and less intense pain after six months, compared with nonparticipants.
Back in 2008, when Smith realized that he should ask people about their discomfort, he launched a new era of research into sickle cell pain. “We discovered this submerged part of the pain iceberg that is pain at home,” he says. “We were only looking at the tip of the iceberg.”
Sixteen years after Gupta heard a young boy talk about his pain and learned of Smith’s study, she says, researchers are pushing the field forward, but pain remains mysterious in many ways. Eventually, experts hope, their science will ease the suffering.