Dolores Perales was 10 years old the first time she couldn't take a breath and thought she was going to die. Parts of the memory remain vague: she knows it was early April, the start of softball season, and she was playing outside. What she remembers clearly is the tightness in her chest and the rising panic. After it happened repeatedly, her mother took her to a doctor, who diagnosed her with asthma. “Ever since then I just had my inhaler,” she says. “One of my younger brothers had asthma; my cousin across the street had asthma. So many of the kids in my classroom had asthma,” Perales says. “As a kid, you kind of start thinking this is something normal.”
Equally normal, as far as Perales was concerned, was a Detroit skyline hazed by the fume-spewing Marathon petroleum refinery. And the Ambassador Bridge—the busiest vehicle crossing between the U.S. and Canada, often packed with idling, diesel-fueled trucks—was typical, too. Both were within a few miles of her home.
It was not until Perales began traveling with her middle school softball, volleyball and basketball teams that she realized the chemical-laced air she knew so well was not the norm for everyone. Just a 30-minute drive from her own neighborhood, Perales encountered quiet, tree-lined streets. But even more striking to her than the greenery was the suburban air. “It smelled different,” she says. “When I was out there, it didn't smell bad.”
Nearly a decade after that first asthma attack, Perales began attending college at Michigan State University, where the air was so pristine that she rarely needed her inhaler. A few years later, during graduate courses in environmental justice, Perales learned that the emissions in the air that made her so sick were a direct result of discrimination—the refinery and the bridge had been placed where they were because, years before, her community had been deemed less important than the well-to-do suburbs and had neither the means nor the political influence to fight back. Air pollution had become concentrated in her neighborhood as one of the side effects of a discriminatory housing practice known as redlining.
Even when a nation's overall air quality is safe, pockets of polluted air may persist—often in areas where marginalized communities live and work. In the U.S., redlining and practices such as building freeways through poorer neighborhoods have exposed some people to much higher levels of pollution than those in adjacent neighborhoods.
“The major sources of emissions of harmful pollutants are often placed, in unfair ways, in communities that are disadvantaged as a result of discriminatory or racist practices or policies,” says environmental health researcher Rima Habre of the University of Southern California.
In countries around the world the burden of poor air quality—and its accompanying health threats—typically falls on lower-income communities, including immigrants, migrant workers and people from other marginalized groups. Any improvements in air quality tend to start in richer neighborhoods. On a global scale, people in high-income countries breathe cleaner air than those in low- and middle-income countries.
Improving air quality is one of the biggest opportunities the world has to save lives and reduce health inequities. In one 2011 estimate, the Environmental Protection Agency predicted that the Clean Air Act would prevent about 230,000 early deaths in 2020 alone. Another U.S.-based study, this one from 2022, estimated that reducing pollution from energy production could save an additional 50,000 lives every year. Such policies could go even further if health equity is factored into policymaking, experts say.
Over the past few decades efforts to learn more about air-pollution risks have led to a greater understanding of the inequity of exposure and how it contributes to health disparities. As Susan Anenberg, an environmental health expert at the George Washington University, says, “We can now get down to a pretty granular scale when thinking about who receives the health benefits of improved air quality and who is still having to deal with the repercussions of poor air quality.”
Downwind Threats
In the 19th century smoke from inefficient coal fires became one of the first signs of increasing wealth as cities and industries expanded. Coal and petroleum products remain among the primary sources of air pollution around the world. In other words, economic growth still taints the air.
In some places, smoke was considered an aesthetic problem but not necessarily a medical one. Most people were “only concerned with that which was visible,” says historian Awadhendra Sharan of the Center for the Study of Developing Societies in Delhi, India. “There's this long-standing view that there is something aesthetically wrong with a polluted atmosphere.”
In the U.S., efforts to protect more privileged communities from ugly emissions pushed the dirty air into neighborhoods like Perales's in southwestern Detroit, which were home to immigrant, Black and Hispanic families. The infrastructure needed to support the city, such as the Marathon petroleum plant and the Ambassador Bridge, had to be placed somewhere, “and that somewhere was here,” Perales says. “This was an area that was considered undesirable.”
It's only in the past 75 years—after events such as the deadly 1948 smog in Donora, Pa., and London's Great Smog, which killed 4,000 people in 1952—that more researchers, physicians and activists began to recognize the health risks of dirty air.
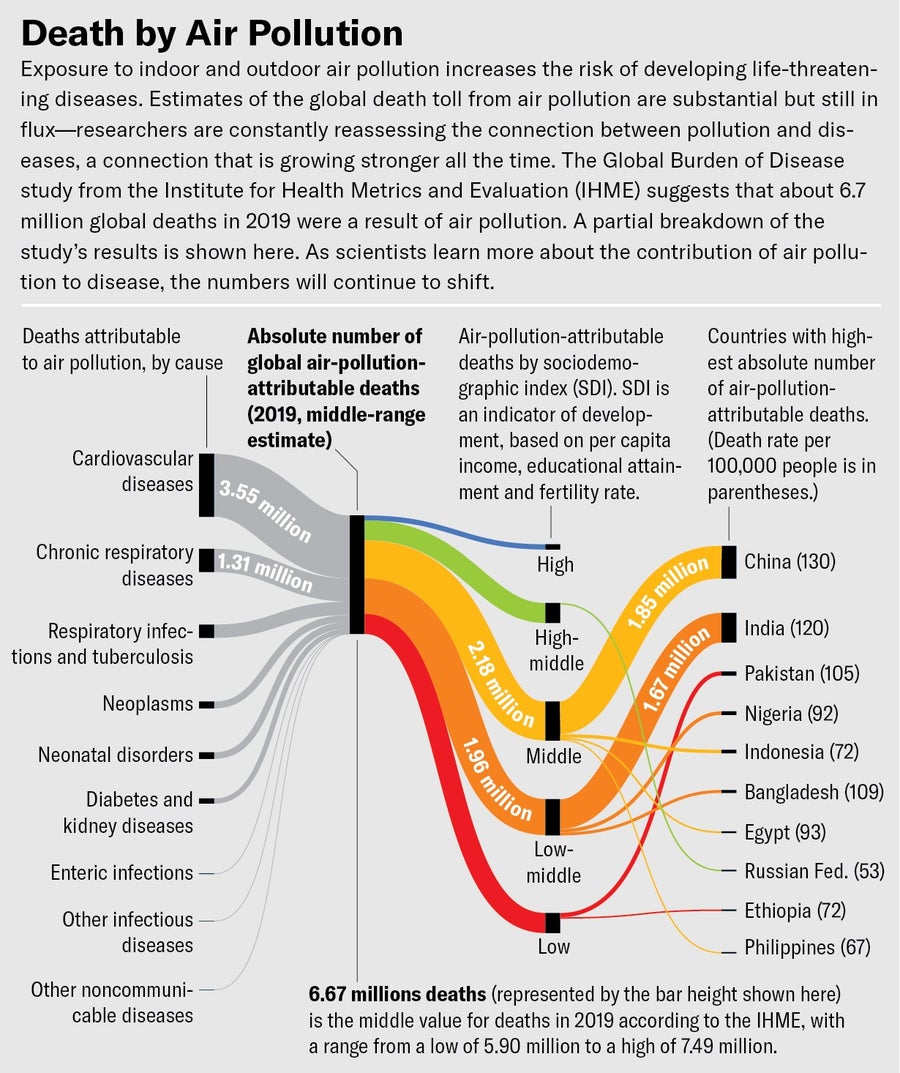
Credit: Miriam Quick and Jen Christiansen; Source: Institute for Health Metrics Evaluation. Used with permission. All rights reserved (data)
Air pollution endangers almost every aspect of human health. The worst threat comes from tiny particles, known as PM2.5, that are 2.5 microns or less in diameter. Once inhaled, they can cause or exacerbate respiratory diseases such as asthma, chronic obstructive pulmonary disease and lung cancer. These minute particles slip through layers of lung tissue to enter blood vessels and affect major organs such as the heart, kidneys and liver. They cause inflammation that touches every part of the body, including the brain, and have been linked to heart disease, neurodegenerative illnesses and even dementia. “It seems as though pretty much every organ system can be affected by pollution,” says environmental health researcher Michael Brauer of the University of British Columbia and the University of Washington.
People who feel the health impacts most keenly are those who live or work near sources of pollution, such as oil refineries, coal-burning power plants or freeways with smoke-spewing trucks. Numbers can swing wildly from day to day, but PM2.5 levels can get six to eight times higher in pollution hotspots than in neighboring areas. “Many of those very local hotspots of air pollution are inequitably distributed, in the U.S. especially, on the basis of race and socioeconomic status,” Brauer says.
Globally, the degree of risk from deadly air correlates with a person's income and social class. The pattern can be seen at every scale, whether looking at the difference in wealth across nations, neighborhoods within a city or neighbors in a small town. When Brauer was conducting studies of air quality in villages across Mexico and India, he could tell which families were most likely to breathe more dangerous air based solely on signs of poverty.
“We see this pattern across the world, and you can even see it within a single village,” Brauer says. He has noticed that poorer families tend to live crowded together in one-room homes. And when the same space is used for cooking, living and sleeping, the entire family is exposed to cookstove fumes. Cookstove fuel differs across classes, too. Poorer families burn crop waste or freshly gathered wood, both of which create more smoke than the dry wood used by wealthier families. In cities, Brauer says, richer people live in homes set back from busy roads, whereas those with fewer means are more likely to live near factories and highways.
Another pattern that researchers see over and over again is that those breathing more toxic air are also those who are most likely to experience societal stressors: poverty, racism, limited health-care access, and more. The combination increases their risk of disease. Researchers are only now beginning to tease apart how the chronic stress of discrimination makes someone more vulnerable to the harms of environmental pollutants. “Social factors cause repeated chronic stress to the point that the body has a harder time defending itself against harmful exposures,” Habre says. People who experience social discrimination, especially based on race or ethnicity, are “getting higher exposures, but they are also more susceptible to their harmful effects.”
Seeking Solutions
According to a 2022 Lancet study, air pollution caused about 6.7 million premature deaths in 2019, mostly in low- and middle-income countries. The nation with the highest number of these deaths was India. As part of its efforts to address this threat, in 2015 the Indian government issued a report that declared air pollution a national health concern. The report laid out a plan to start improving the nation's air, one of the first of its kind from a low- and middle-income country that, Sharan says, clearly states “it is exposure to emissions that matters, and therefore the people who are exposed to it that matter. Once you do that,” he says, “then the question of equity comes up.”
Creating policies that protect and prioritize the health of the most vulnerable is far from easy. In New Delhi, for instance, air quality is especially awful during certain winter months because of local weather conditions and emissions from agricultural burning as farmers clear fields for planting. To try to protect people's health, government authorities identified a set of steps they hoped would reduce toxic air exposure in the nation's capital. When PM2.5 levels hit a certain mark, schools are to shut down so children can stay indoors. Vehicles must drive only on paved roads so as not to throw excess dust into the air. Private construction activities—at homes, malls, and other nonessential sites—must halt to protect workers and reduce the amount of fine particles flying into the air from cement grinding or stone cutting.
These steps can temporarily lower local PM2.5 levels. But the cost of this reduced activity is most keenly felt by laborers who are paid daily wages. When schools are closed, children in poorer families are more likely to spend time outdoors than to remain inside next to an air purifier.
The people who can't afford to pay attention to the health risks of PM2.5 are typically those most at risk. Thus, when a policy to reduce exposure to pollution threatens someone's income—or a country's economic development, for that matter—it's likely to fail.
Policies that work in rich countries can prove challenging to implement in low- and middle-income nations. Pallavi Pant, a global health researcher at the Health Effects Institute in Boston, points to car emissions as one example. In Kenya and Uganda, the demand for personal vehicles has led to an increase in imported used cars from countries such as Japan. These imported cars were designed to meet emissions-control standards for high-income countries, so they're built using the newest catalytic converters and other pricey pollution-reducing technology. But maintaining those cars, especially locating and paying for parts, can prove difficult in poorer countries. As a result, importers have taken to removing these components altogether before the cars are resold.
But top-down approaches may still be effective, Pant says. In India, for instance, regulators have begun to enforce more stringent standards for vehicle emissions, an approach shown to motivate the auto industry to find ways to meet those standards so it can continue selling cars. The results from this strategy are not yet visible, Pant says, because it takes time for an older fleet of vehicles to be replaced by new, cleaner ones. “We'll continue to see improvements in the vehicle fleet,” she says.
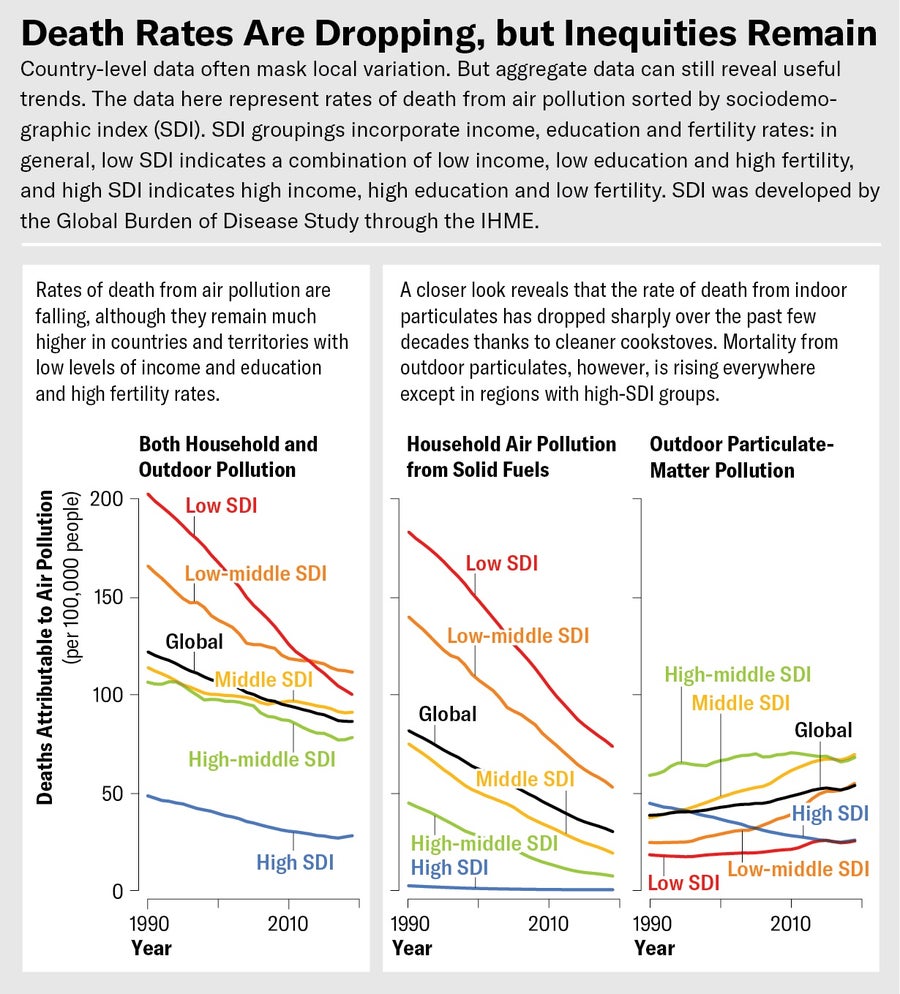
Credit: Miriam Quick and Jen Christiansen; Source: Institute for Health Metrics Evaluation. Used with permission. All rights reserved (data)
The Indian government has also implemented the National Clean Air Program, a 2019 initiative that tasks state and municipal authorities with especially dirty air to find solutions to their pollution problems. The effort empowered local governments to begin acting on their own air pollution—perhaps most important by making funds available to implement solutions. “That has been a pretty pivotal shift,” Pant says. “There's a lot more still to do, but it's a very useful first step in getting people involved.”
By themselves, policies and laws cannot tackle the many ways that pollution from high-income countries is exported to low- and middle-income countries, Brauer says. Morals matter, too. He and his colleagues have quantified how outsourcing the production of consumer goods and services from the U.S. to Asia also outsourced the pollutants created by those factories. They estimated that, for the year 2007, about 22 percent of the 3.45 million deaths attributable to air pollution were a result of this reassigned burden of pollution. Although the data are now 15 years old, they still point to an important message. People should be “aware that some of what we are benefiting from has just been transferred to other people,” Brauer says.
Progress without Pollution
In wealthy countries, air quality has been improved in part by new, expensive technologies that reduce pollutants but still rely on petroleum and other fossil fuels. Over the long term, however, such a strategy cannot fix the entire problem, because it does not minimize greenhouse gases, which also harm human health and are accelerating the climate crisis, Anenberg says. “We need to be simultaneously reducing greenhouse gases and air pollutants. And the way we do that is by burning less fuel, not putting on these technological control measures.”
For decades industrial growth and the amount of pollutants in the air rose and fell together, Brauer says. Although pollution typically settles on the poorest, one exception is in countries with little industrialization, which still have relatively clean air. But as they industrialize and increase their reliance on fossil fuels, their air quality begins to worsen. “We've gone through this in high-income countries,” Brauer says. “But many low- and middle-income countries are still in the earlier phases of this arc of industrial development.”
Recognizing this problem has prompted some low- and middle-income countries to make changes. Rwanda, for example, has focused on off-grid solar-powered systems to provide electricity to rural areas. As of 2021, nearly 50 percent of the country had access to electricity, with much of that a result of solar power. India, too, is working to increase the amount of electricity it gets from renewable sources. In May the Indian government announced plans to pause proposals for new coal-burning power plants for the next five years and focus instead on renewable energy. “It's not a case that places get worse and worse and never improve,” Brauer says. “We really do see improvement.”
Such improvements happen when nations prioritize clean air and healthy citizens over short-term profits. Some high-income countries have introduced stringent policies to control pollution that have already led to measurable health improvements. In the U.S., one estimate found that laws controlling vehicle exhaust lowered mortality from traffic-related PM2.5 by 2.4 times between 2008 and 2017. In London, the creation of an ultralow-emission zone in the central part of the city has reduced the amount of sick leave by an estimated 18 percent.
Another way to offset the health effects of pollution and simultaneously clean up some of our environmental mess is through planting trees. Exposure to PM2.5 can significantly reduce blood flow to the brain, which influences stroke risk. But a study tracking more than 9,000 residents in Beijing found that living amid greenery mitigated this potential harm. And other research has shown that plants might also minimize heart disease risk from PM2.5.
Today, armed with cleaner technologies and an awareness of toxic air's deadly effects, there's a chance that less industrialized countries could continue to choose progress without pollution. “This is not an either-or situation,” Anenberg says. “We can do both of these at the same time.” For clean and healthy air, this may be the only way to achieve true equity.
This article is part of “Innovations In: Environmental Health Equity,” an editorially independent special report that was produced with financial support from Takeda Pharmaceuticals.
