This article was published in Scientific American’s former blog network and reflects the views of the author, not necessarily those of Scientific American
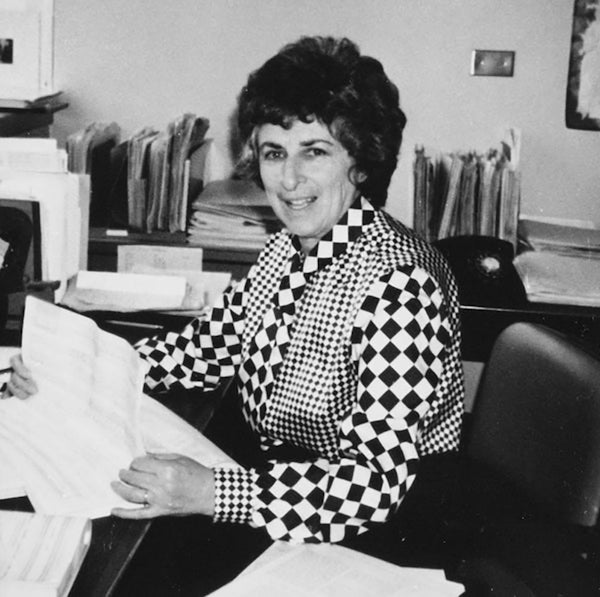
It is a regrettable fact that science has historically undervalued the contributions of women. Elizabeth Stern is probably one of the most significant physician-scientists who worked at the interface of epidemiology and cancer in the mid-20th century, but it is unlikely you have ever heard her name. You won’t read about Stern’s research in medical textbooks, or find any symposiums or departments dedicated to her memory. But her groundbreaking research led the way to our modern understanding of the prevention, diagnosis and treatment of cervical cancer.
Elizabeth Stern was born September 19, 1915 in Cobalt, Ontario. She was the fifth of eight children born to George and Sarah Stern, who emigrated from Poland to escape growing anti-Semitism and political unrest in Eastern Europe. She graduated from the University of Toronto School of Medicine on June 8, 1939, at the age of 23. While at the University of Toronto she met Solomon Shankman, a doctoral student in chemistry, and they married in 1940. They soon immigrated to Los Angeles, California, where Stern completed residency training in pathology at Cedars of Lebanon and Good Samaritan Hospitals in 1946.
From 1950 to 1960 she served as the director of laboratories and research at the Los Angeles Cancer Detection Center. In 1961 Stern was hired by the University of California Los Angeles (U.C.L.A) School of Medicine as the chief of the Cytology Laboratory, and began her research lab in the Department of Pathology. In 1963 her laboratory was transferred to the U.C.L.A. School of Public Health. Stern’s former colleague and distinguished cytopathology expert Dorothy Rosenthal commented that, “The Department of Pathology didn’t want to keep [Stern] … because the Chair did not want to fill a full-time faculty position with a cytopathologist.”
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
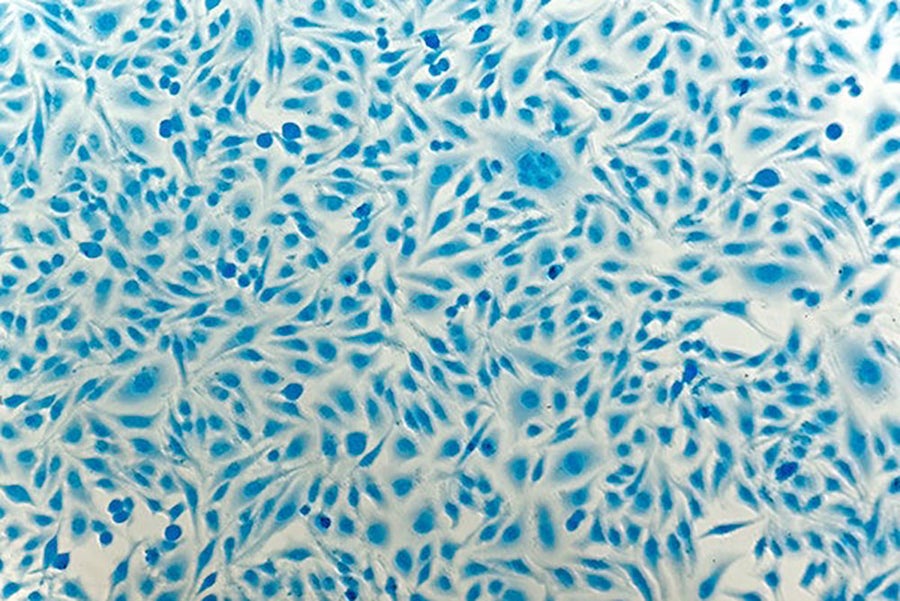
Cervical cancer cells under the microscope. Credit: HeitiPaves/Getty Images
Cytopathology refers to the diagnosis of disease at the cellular level. The first cytopathology tool widely used in the United States was the Pap smear test, which was adopted in the 1950s to screen patients for cervical cancer. The Pap test has helped reduce cervical cancer frequency and mortality by more than 70% compared to the 1950s. However, few physicians in the 1960s were interested in further research connecting cell shape and morphology to disease. As Rosenthal remarked, “The field of cytopathology at the time was fledgling. A lot of people in pathology, and medicine in general, looked at it as if it were witchcraft.”
One of Stern’s primary research interests was the role of dysplasia in the development of cervical cancer. Dysplasia is abnormal cell growth that is non-invasive to surrounding tissues, and often reverses back to normal epithelial morphology. In the 1950s and 1960s the early stages of cervical cancer were not well defined, and although dysplasia was noted in smear results, it wasn’t considered a cause for concern. But what if dysplasia was indicative of something more serious? Stern hypothesized that these morphological abnormalities could be an early sign of cervical cancer development.
To investigate this question, Stern and her group organized long-term epidemiological studies, in one report collecting Pap test samples from over 10,000 women in Los Angeles County. They carefully documented results of patients at the beginning of the study, and again at follow-up tests performed over the course of the seven-year study. She found that patients diagnosed with dysplasia at the start of the study were at significantly higher risk for cervical cancer. Stern would go on to lead over a dozen epidemiological studies providing nearly irrefutable proof that dysplasia is an early marker of cervical cancer.
It’s difficult to overstate how important this discovery was to the medical community, and how innovative her theory was at the time. Today dysplasia is identified during routine cervical cancer screenings using the Pap test, and patients are monitored closely for further progression to carcinoma. The idea that dysplasia could possibly be seen as a debatable risk factor for cancer is preposterous today, largely due to Stern’s meticulous and groundbreaking research.
Of all of Stern’s achievements, perhaps her most lasting legacy is in the modern technology of the Pap test. She collaborated with the Jet Propulsion Laboratory (JPL) and Rosenthal, then the head cytopathologist at U.C.L.A, to apply NASA computer imaging technology to Pap screening. Stern developed a liquid-based sampling system to isolate and enrich the cervical epithelium, and helped define cellular criteria for computer programs. The work she did at JPL revolutionized Pap screening for cervical cancer, and her liquid-based sampling technique is still used in hospitals, laboratories, and clinics around the world.
Stern was also interested in other risk factors related to cervical cancer development. By again combining epidemiological analysis with cytopathology, she found that the original high-dose estrogen birth control pill increased the rate of cervical cancer six-fold. She testified to FDA advisory committees about this risk, and her research was quoted in news articles at the time on the questionable safety of 1970s era birth control pills. Her efforts were essential in prompting drug companies to reformulate birth control pills to protect women’s health.
One of the reasons Stern’s work was so comprehensive was her persistence in finding and screening at-risk women. Few researchers succeeded in recruiting at-risk populations, or enrolling them in high enough numbers to have reliable results. Stern’s group published some of the earlieststudies documenting the difficulties of poor women accessing preventive medical care, and demonstrated that providing help, such as childcare or transportation, can increase life-saving care to high-risk populations.
Stern continued working on her research after she was diagnosed with stomach cancer, and was writing manuscripts until her death in August 1980. In remembering Stern, I see someone that served as a strong and inspiring role model for countless women scientists. Stern had a challenging start at U.C.L.A. Her daughter Janet Williamson recalls that, “As a woman it was a struggle … the first year she worked at U.C.L.A. she was not paid a salary.” Through her perseverance she changed the way doctors diagnose cervical cancer, and shaped the field of cytopathology for decades to come.
Stern was a true embodiment of women in science. One of my favorite memories of Stern is from Marilyn Winkleby, a renowned epidemiologist at Stanford University, who credits Stern’s lab for starting her research career. “I remember her being alone in her office working on her science. That’s the picture I have of her. Sitting right outside her busy basic science lab. But the door was always open; the door was never closed.”