Shantaquilette Carter-Williams was on the gym treadmill when she first felt an odd flutter in her heart. “I remember stopping and thinking, ‘That doesn't feel right,’” says the now 43-year-old Dallas resident. But she knew the importance of exercise—she walked or ran almost every day—so she got back to it and finished her workout.
She followed up with a doctor who diagnosed her with exercise-induced arrhythmia and told her to be careful with increasing her heart rate, says Carter-Williams, a retired accountant. She switched to different kinds of workouts. That was in 2012. Over the next six years worrying symptoms such as chest pain took her to the emergency room a dozen times. Each time doctors there sent her home with no diagnosis and no way to prevent it from happening again. In June 2018 lingering back pain, stomachache and nausea led Carter-Williams to think she had the flu. She was working from home and planned to go to bed early, instead of making another inconclusive trip to the hospital. She was just wrapping up a phone call when her college-aged daughter stepped into the room. Carter-Williams turned to speak, and a bizarre pain shot down the left side of her jaw and neck. “I'd never felt anything like it before,” she says.
Her daughter drove her to the hospital. As they waited to be seen, Carter-Williams began to vomit. An intense pressure, “like someone stepping on my chest,” overwhelmed her. She was handed a pill to place in her mouth. Then her heart started to race. She remembers that hospital staff gave her an injection in her belly and administered other drugs. A brown-skinned doctor came into the room shortly after. He leaned over, held her hand and said, “I don't want to scare you, but you're having a heart attack.”
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
After the specialist left, her own cardiologist, who was a resident at the hospital, took over her care. She was discharged a few days later with no medication to prevent another incident—contrary to common clinical recommendations. As it turns out, that's not an uncommon situation. “Unfortunately, guideline-based therapies are not uniformly applied to all patients,” says Roxana Mehran, a cardiologist at Mount Sinai's Icahn School of Medicine in New York City. “Women and underrepresented minorities are less often treated with guideline-directed medical and interventional treatments.”
Nine months later, at age 40, Carter-Williams had a stroke.
As a Black woman, Carter-Williams was at high risk of having a heart attack. Despite that, she is also among the patients most likely to be overlooked in screening tests or have symptoms dismissed as not heart-related. Outdated thinking holds that overeating or a sedentary lifestyle are the main risk factors. But discrimination is also deadly: both within the U.S. and around the world, people who experience gender, race, socioeconomic or other discrimination are far more likely to suffer and die from heart disease.
Understanding of heart disease has dramatically expanded over the past half a century. In the 1940s heart disease caused around half the deaths in the U.S. The epidemic precipitated a flood of research that resulted in landmark, lifesaving discoveries. Researchers found, for example, that inactivity, smoking, alcohol consumption, and diets rich in fatty foods or salt raised a person's risk of heart disease. They discovered how conditions such as diabetes and high lipid levels increased the chances of heart attack or stroke and designed drugs to stave off these dangers. And for those who wound up in emergency rooms despite these measures, surgical advances such as balloon catheters, stents or artificial valves made heart attacks less deadly.

The three children of ShantaQuilette CarterWilliams place their hands over their mother’s heart. Credit: Gioncarlo Valentine
Over time deaths dropped—at least in higher-income, majority communities in industrial nations. But as research on cardiovascular disease risk adopted a more global approach, heart disease again emerged as the number-one killer worldwide. These new studies revealed that the same risk factors drove heart attacks no matter where a person lived or what their socioeconomic status was. The difference was that now about 80 percent of heart attack victims lived in lower- and middle-income countries.
“For far too long, we didn't have high-quality studies of cardiovascular disease that included people” from lower- and middle- income countries, says Amitava Banerjee, a cardiologist at University College London. Within the U.S., research centered on higher-income communities. And in the rest of the world, the focus was more on the differences between Western and Eastern countries than on their similarities—something that, Banerjee says, stems from “a history of colonialism in medicine” that aimed to serve expats instead of local communities.
Now researchers have focused on bridging these gaps. They are showing that, at every level, advances in reducing the burden of heart disease are less likely to reach or help people who experience discrimination. Long-standing biases have resulted in medical treatments that are less available or, when available, less useful to historically marginalized communities. Not only do these people face barriers of access, they are also often disproportionately burdened by risk factors such as air and water pollution.
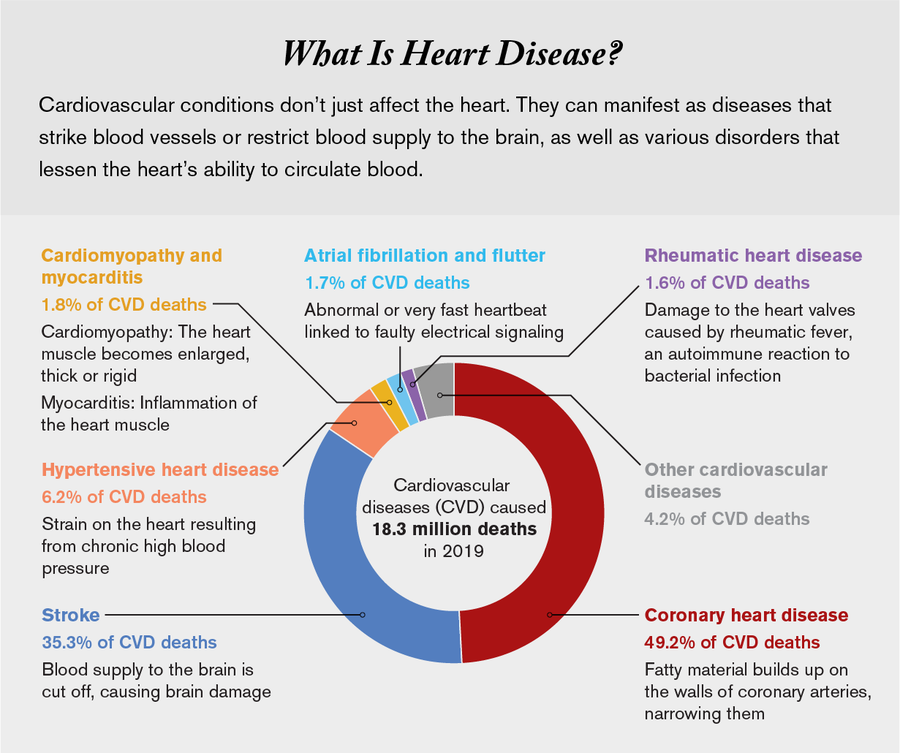
Credit: Amanda Montañez, Research by Miriam Quick; Source: Institute for Health Metrics Evaluation. Used with permission. All rights reserved. (data)
The biology of heart disease is universal. Tests, drugs, and other interventions for reducing heart attack risk are the same everywhere in the world. Despite this shared foundation, solutions addressing the problem were mostly developed within a limited, Western context. They fail to account for social circumstances that can make diagnostics, preventive medicine and treatments inaccessible to the rest of the world. “We can't just transport what we find in high-income countries and assume it's going to work in low-income countries,” says Shivani Patel, a social epidemiologist at Emory University. “There are powerful social influences that need to be included in the constellation of risk factors.”
Overlooked and Underrepresented
In 1947 the U.S. Public Health Service (now the National Institutes of Health) launched a study that tracked both the health and life habits of residents of the town of Framingham, Mass., and then looked at how those corresponded to heart health. Thanks to the Framingham Heart Study—which continues today—and others conducted in the U.S. and Europe, clinicians now know precisely how heart disease begins, worsens and kills. And they know, to a great extent, how to stop it.
In 1990 William Kannel, a former director of the Framingham Study, gave a lecture in which he reported that the study linked heart disease to a “lifestyle typified by a faulty diet, sedentary living, unrestrained weight gain and cigarette smoking.” Therefore, people could improve heart health by changing how they lived. Public health campaigns around the world spread the message. In the U.S., the American Heart Association launched a campaign, called Life's Simple 7, defining seven different things—such as smoking, diet and physical activity—that could decrease cardiovascular risk.
Despite the name, these measures are anything but simple. The advice to eat healthier foods and be physically active is rooted in strong evidence, but it does not account for people around the world whose lives look nothing like those of the mostly white, mostly well-off residents of a Boston suburb. “The current recommendations have fallen short because of the lack of focus on social determinants of health and structural drivers” that influence a person's health practices, says LaPrincess Brewer, a cardiologist at the Mayo Clinic in Minnesota. “Unfortunately, Life's Simple 7 aren't necessarily delivered in the [appropriate] sociocultural context.”
Consider exercise. Even when feasible, it is not enough by itself to ensure a healthy heart. Carter-Williams knew exercise was important, particularly because her job came with a lot of desk time. But a treadmill habit wasn't enough to prevent her heart attack. For others, just walking out the door is a difficult ask. A lack of access to safe spaces for exercise, smog-filled air or cultural barriers to women walking alone frequently hinder or prevent physical activity. Patel points to India as an example, where persistent colorism drives women, particularly adolescent girls, to stay indoors (and thus be less active) to prevent sun-darkened skin.
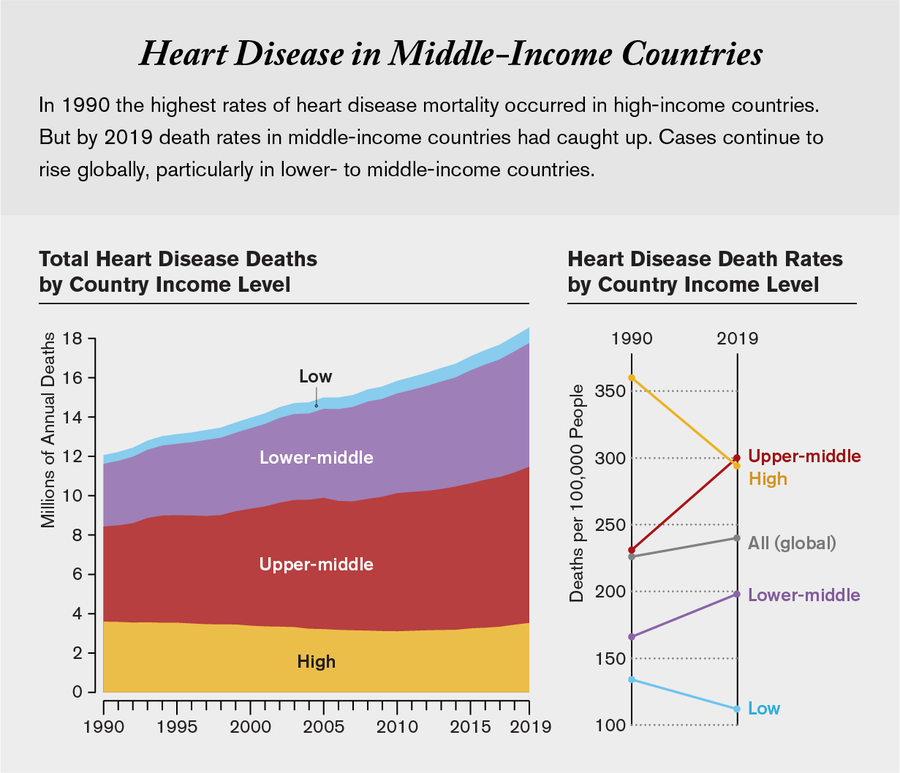
Credit: Amanda Montañez, Research by Miriam Quick; Source: Institute for Health Metrics Evaluation. Used with permission. All rights reserved. (data)
Other times recommending exercise is simply absurd, says Andre Pascal Kengne, an internist and researcher at the South African Medical Research Council. In rural areas of South Africa, he points out, people at risk of heart disease often work physically demanding jobs, making planned exercise superfluous: “Think of a farmer who spends six to eight hours a day working on a farm,” he says. “If you tell him at a consult to exercise, what do you expect to achieve?”
Western dietary recommendations also fail to account for how diets vary by culture. So-called heart-healthy foods described in public campaigns reflect a small subset of norms from industrial nations while excluding most culinary traditions around the world, including in the U.S. Public campaigns aim for awareness, but Brewer points out that the problem for most people is not a lack of understanding or knowledge.
Translating awareness into a change in habits is stymied by many factors: a lack of culturally relevant guidelines, financial insecurity or an inability to access affordable, nutritious food. “Whether it's their ability to place food on the table or lack of outlets to purchase healthy food,” Brewer says, community members are aware they face these issues. The problem, she says, is that they find it tough to act on diet or exercise recommendations given their financial or social circumstances.
Around the world, people of low socioeconomic status or those who live in food deserts are the most likely to have diets high in sodium and saturated fats and low in fresh produce. In a study of 195 countries published in the Lancet, researchers found that such diets remain the leading cause of heart disease. People eat this way out of necessity, not choice. “The reality is that wherever you are, the cheapest way to eat is often the least healthy,” Banerjee says. Across the world, highly processed foods have grown more common and accessible—more so than fresh fruits and vegetables—at least in part due to subsidies that often make junk food cheaper even in the poorest communities.
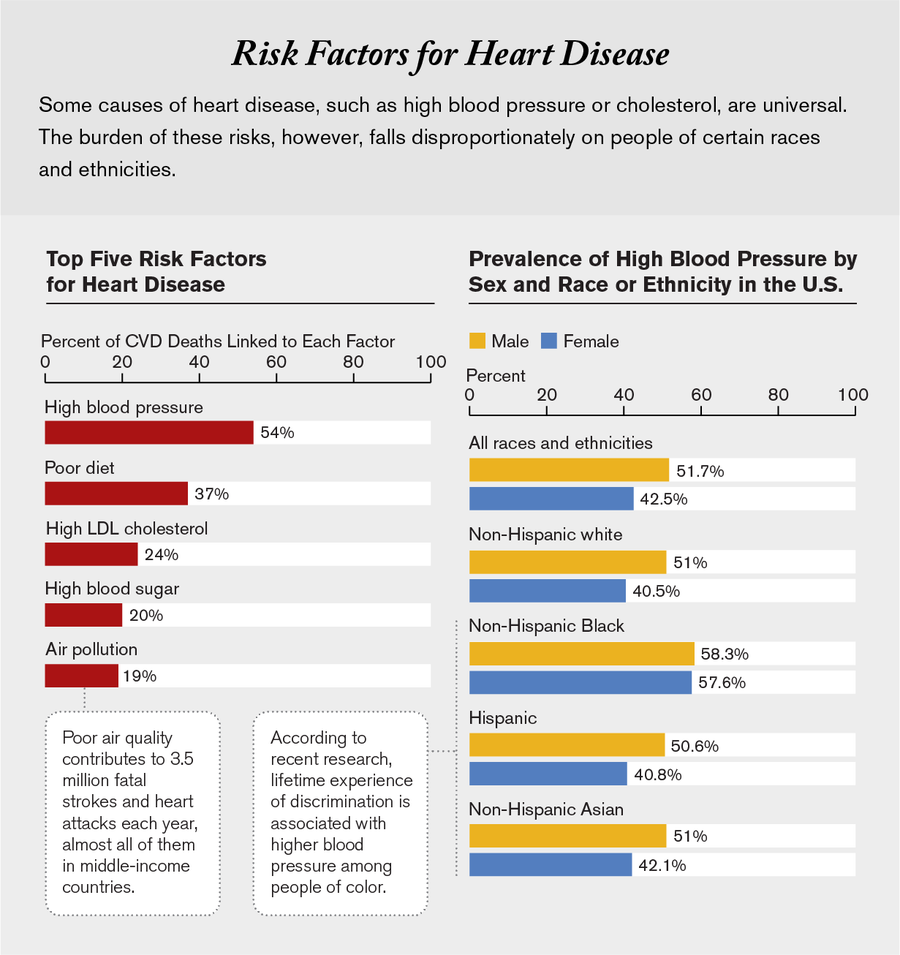
Credit: Amanda Montañez, Research by Miriam Quick; Sources: Institute for Health Metrics Evaluation. Used with permission. All rights reserved. (risk factor data); “Heart Disease and Stroke Statistics—2022 Update: A Report from the American Heart Association,” by Connie W. Tsao et al., in Circulation, Vol. 145; February 22, 2022 (hypertension prevalence data)
In many low- and middle-income countries, rates of obesity and diabetes initially rose fastest in urban areas. Now rates are rising in rural areas as well, Patel says. These shifting trends, which are likely to result in more instances of heart disease, mean the condition has moved firmly beyond being a disease of affluence or sedentary lifestyles associated with city living.
Patel spent a few years in the village of Juna Mozda, in the western Indian state of Gujarat, and now focuses on understanding heart disease risk factors in communities across the country. Most of Juna Mozda's residents are Adivasis, members of tribal communities. “Some of the highest rates of high blood pressure are among these Indigenous communities, who are often the poorest,” Patel says.*
Ishwar Vasava, a farmer and social activist who has lived in Juna Mozda all his life, says he has noticed a shift in people's diets over the years: more sugar spooned into tea, traditional grains replaced with rice, and desserts and fried treats now a part of daily routines. Alcohol use is a concern, too, Vasava says, especially in young men who return to the village after years of working in adjacent industrial towns. “I don't see much of a difference between our life in the village and that of the city anymore,” he says.
Urban or rural, simply telling people to eat better and drink less alcohol is unlikely to address rising rates of cardiovascular disease. “We tell the story that people can change their risk themselves,” says Joel Kaufman, an epidemiologist at the University of Washington. “But people can't change their diet and lifestyle as much as we'd like to think.”

Shown clockwise with their mother, ShantaQuilette, and father, Roy Williams, are daughters Sanaa and Nyaira and son Adysaan. Credit: Gioncarlo Valentine
Biased Benefits
In high-income countries, lifestyle-based changes have clearly helped cut rates of heart disease: Smoking bans, awareness campaigns and other policies limiting tobacco use have made large contributions to the decrease in deaths from cardiovascular disease. So have advances such as better screening tests and prescription drugs. Medications for treating diabetes, hypertension, high cholesterol, and other conditions have proved so effective that they are now on the World Health Organization's list of essential medicines for all countries.
The blood tests most often used to prescribe these drugs unfortunately do not work equally well for everyone, because they were developed using data from men of European ancestry. The hemoglobin A1C test for diabetes (which, untreated, is a risk factor for heart attacks) does not work for people who are of Asian or African descent if they are anemic or are not overweight. And the most commonly used cholesterol and triglyceride assessments do not work as well to assess risk among Black individuals in the U.S. Even when test results show normal levels of triglycerides, statistics from the Centers for Disease Control and Prevention show that Black people experience higher rates of hypertension than white, Hispanic or Asian groups, says Anne Sumner, an endocrinology researcher at the National Institute of Diabetes and Digestive and Kidney Diseases. “Health disparities are not just related to not having access to care. You have to have access to the right screening tools, too.”
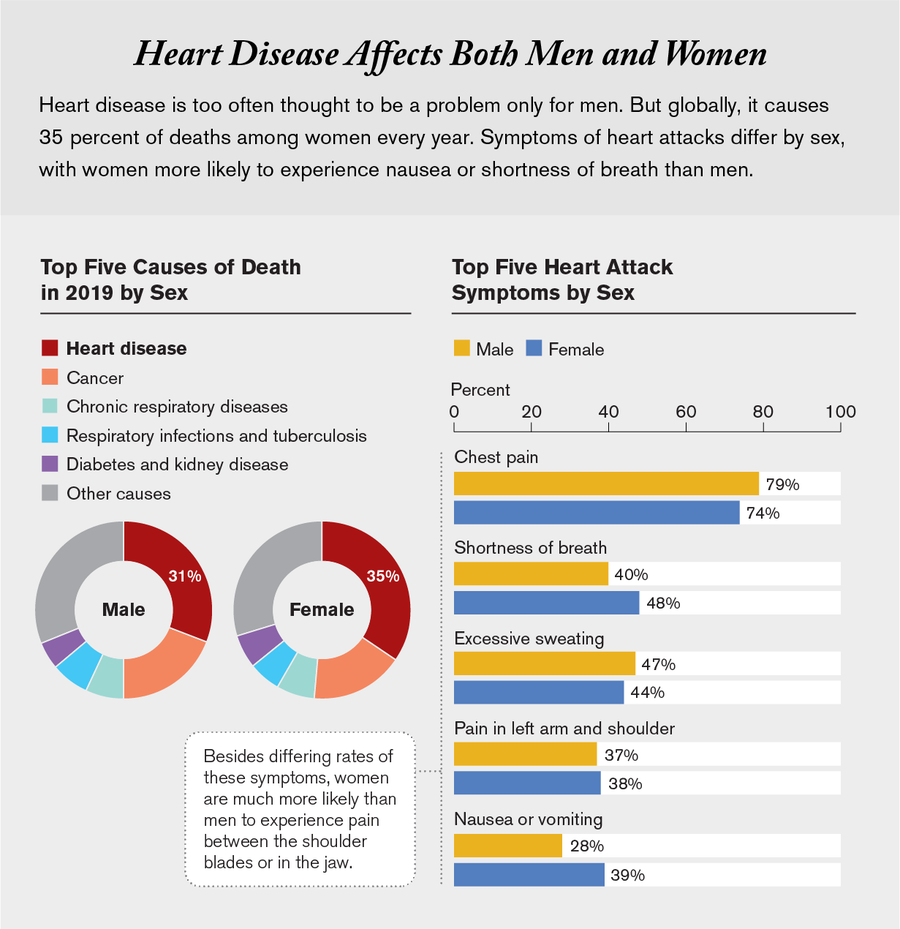
Credit: Amanda Montañez, Research by Miriam Quick; Sources: Institute for Health Metrics Evaluation. Used with permission. All rights reserved. (death rate data); “Sex Differences in Symptom Presentation in Acute Coronary Syndromes: A Systematic Review and Meta-Analysis,” by Roos E. M. van Oosterhout et al., in Journal of the American Heart Association, Vol. 9; May 5, 2020 (heart attack symptom data)
Precisely how much harm is caused by inaccurate screening tools is tough to know for certain. Shortly after her heart attack, Carter-Williams looked through her old medical records and found some numbers highlighted as abnormal. When she asked her doctors about the results, she says, “they really could not give me an explanation other than ‘it's not high enough for us to be concerned.’” She only began to receive cholesterol medication 10 months later, after her stroke.
Even when test results are accurate, barriers to treatment persist, particularly in low- and middle-income countries. It can prove nearly impossible for some people—like the farmer who spends his days doing manual labor—to get to a clinic in the first place. In South Africa, subsidized health care ensures that patients at many clinics do not pay for preventive drugs, says Kengne of the South African Medical Research Council. “If they can get to the clinic, the medication is free,” he says. “But the transportation cost to get there” is the problem.
The cost of medications as well as their availability hinders access to drugs in many low- and middle-income countries. In a 2020 study of 21 countries published in BMJ Global Health, researchers linked the inaccessibility of necessary medicines to higher odds of disability and death from heart disease. Drugs that treat diabetes or hypertension are available to only about 50 to 60 percent of the population in both high-income countries and low- and middle-income countries. In the latter case, a month's worth of brand-name medication typically costs six days' wages, whereas generics cost about two days' worth. “The most common reason people give me for stopping their medicines is financial,” says Jaideep Menon, a cardiologist at the Amrita Institute of Medical Sciences and Research Center in Kochi, India. “Another is because the drugs aren't available in a pharmacy near them.”
Gender, age, caste and socioeconomic status all determine who gets care, Menon says. Discrimination based on these factors results in what researchers call “social deprivation”: restrictions in a person's ability to access health care.
Those biases are not limited to low-income countries. They frequently prevent access to quality care in high-income countries, too, particularly if someone is Black or female. “The places where we start to see a gender divide and increased heart disease rates in women” is in places where they experience discrimination, says Mount Sinai cardiologist Mehran. “That includes right here in the U.S., where there's discrimination against them based on income, education, and other factors.”
Women in cardiac distress are less likely to be noticed or given timely care. Heart disease and stroke cause 35 percent of deaths in women, but their symptoms are different from men's, and surveys show that physicians are less confident diagnosing heart attacks in women than they are in men. They are more likely to attribute a woman's heart attack symptoms to stomach upset or mental health issues. And women—particularly young Black women—are less likely to receive treatment, either preventive or once a heart attack has already occurred.
For her part, even after she had been diagnosed with cardiovascular issues, Carter-Williams was told nothing was wrong and to “stop stressing out over her job,” she says. She was never tested for blocked blood vessels, something that increases someone's odds of another heart attack. Despite a family history of heart disease and earlier blood tests showing high cholesterol levels and elevated blood pressure, she received no prescription medications.
Nine months after her first hospital stay, Carter-Williams collapsed at work, unable to walk or remember her name. This time the hospital physician suspected seizures. Carter-Williams and her husband were not convinced. After she was discharged, the couple found a new neurologist, a Black woman, who diagnosed her as having had a stroke.
The stroke left Carter-Williams unable to walk or keep up with her job. She took early retirement at the age of 42. And although she is on the mend, she has also taken steps to reduce her odds of experiencing discrimination. After eight years of missed diagnoses, she says, “I fired every one of my doctors who didn't look like me.” Her new care team are either Black or members of other minority groups, she says. “I wanted people who could understand that there is bias.”
Ground Realities
Inequity endures because it is rooted in so many sources: unconscious and conscious bias, centuries of racism marginalizing people of color, a history of forcing those of least means and power into environments that are the most polluted.
That legacy remains a reality for people of color or low socioeconomic status around the world. Research on social determinants of health lags behind progress in drug development for diabetes and hypertension. Starting in 1988, 40 years after the Framingham study began, researchers launched three similar efforts to understand high rates of heart disease in Black, Hispanic and Native American communities. Over the years these and other studies have begun to reveal the importance of discrimination as a risk factor for disease. One study in 2017 in JAMA Internal Medicine found that Black people who lived in more segregated neighborhoods experienced greater rates of hypertension. When they moved to less segregated communities, their blood pressure improved.
“Segregation is a good proxy for a lot of the things we think of when we think of structural racism, including education, earning potential and wealth,” says Kiarri Kershaw, the social epidemiologist at Northwestern University who led the work. The brunt of discrimination is borne out in other research, too. Studies in Brazil, the U.S. and other countries have shown that people who experience everyday discrimination, such as being passed over for a promotion or being harassed by neighbors, tend to have higher rates of hypertension. These social experiences are layered over long-standing regulations and policies that exacerbate inequity. Discriminatory practices in housing and the development of freeways, mines or factories usually result in low-income neighborhoods or marginalized communities bearing the impact of both air and water pollution.
Food policy is similarly biased. Governments in many countries impose lower taxes on the sale of highly processed foods such as refined sugar or oils. Recipients of government subsidies—who are usually poorer—are more likely to consume such products. They are also less likely to be able to afford medicines for chronic conditions such as hypertension or diabetes that result from excess consumption of these foods. Funding to improve medical care for these precursors to heart disease has failed to keep up with the surge in cases, in part because the burden of infectious diseases has yet to wane.
Changing the social and political systems that exacerbate heart disease is a complex, unwieldy process. Global policies continue to prioritize economic development over the health of the most vulnerable communities in the world. Which means, Menon says, “marginalized groups tend to lose out on all fronts.”
This article is part of “Innovations In: Health Equity,” an editorially independent special report that was produced with financial support from Takeda Pharmaceuticals.
*Editor’s Note (5/20/22): This paragraph was edited after posting to update the description of Shivani Patel’s work in India.