As figures emerge about the disproportionate toll that COVID-19 is taking on people of colour in the United States, scientists are suggesting measures to help mitigate the inequalities.
They say that better data are needed on the incidence of the disease, that testing needs to be ramped up and that hospitals serving people at-risk need to better prepare. Researchers and some US lawmakers are now calling for a national commission devoted to identifying racial disparities in health that would act as a unified voice in trying to overcome them.
Researchers note that this will be important to stopping the disease’s overall spread. “It is a major health-disparities issue, but it's also a major health issue for all,” says Cato Laurencin, an orthopaedic surgeon and biomedical engineer at the University of Connecticut in Farmington, who led a roundtable discussion on diversity at the National Academies of Science, Engineering and Medicine.
On supporting science journalism
If you're enjoying this article, consider supporting our award-winning journalism by subscribing. By purchasing a subscription you are helping to ensure the future of impactful stories about the discoveries and ideas shaping our world today.
This is not solely a US problem—an analysis of UK national health records published in May showed that black residents and those of Asian descent were at a higher risk of dying from the virus than were white people—but the disparities are harshly felt in the United States, which currently has the highest number of COVID-19 infections and deaths.
Endemic problems
The US Centers for Disease Control and Prevention (CDC) started releasing death and infection rates broken down by race and ethnicity in late April, only after a public outcry from lawmakers, doctors and civil-rights groups.
The breakdowns were available for just 35% of US deaths. But as these and other data have started to come in, they paint a stark picture of disproportionate disease burden.
As of early May, New York City reported more than twice as many deaths per 100,000 residents for African and Latino Americans than for white people. The city’s highest rates of hospitalization and death occurred in the Bronx, the borough with the highest proportion of African American residents. In Michigan, black people account for 32% of COVID-19 cases and 41% of deaths. They make up just 14% of the population.
Many of the causes for these health disparities are systemic and well known. “We’re getting infected more because we are exposed more and less protected,” says Camara Phyllis Jones, an epidemiologist at the Rollins School of Public Health at Emory University in Atlanta, Georgia. Existing socio-economic and health disparities—caused by historical segregation and endemic racism in the United States—can at least partially explain why people of colour are getting sick and dying at disproportionate rates.
In many parts of the United States, people of colour make up a higher proportion of some low-paid professions that have elevated risks of exposure to the virus—those who staff grocery stores, drive buses and work at food plants, for example. Also, COVID-19 is deadlier for people with chronic conditions, including diabetes, obesity and cardiovascular disease. These have a higher incidence in many minority ethnic and racial groups.
Some say a delayed and flawed federal public-health response is at fault. “That’s because our nation has abdicated its responsibility to do that kind of work, and ask those kinds of questions,” says Jones.
Reaching for solutions
At the earliest stages of the epidemic, aspects of the US response might have made things worse, says Enrique Neblett, a psychologist who studies race and health at the University of Michigan in Ann Arbor. With limited tests available, US authorities initially reserved them for people with symptoms who had a recent history of overseas travel. This could have excluded people from disadvantaged socio-economic backgrounds, including people of colour, says Neblett. “By having that as a criterion they’re automatically less likely to be tested.” Looking ahead, adapting the approaches to getting tests to the people and communities that are most at risk should be a priority, he says.
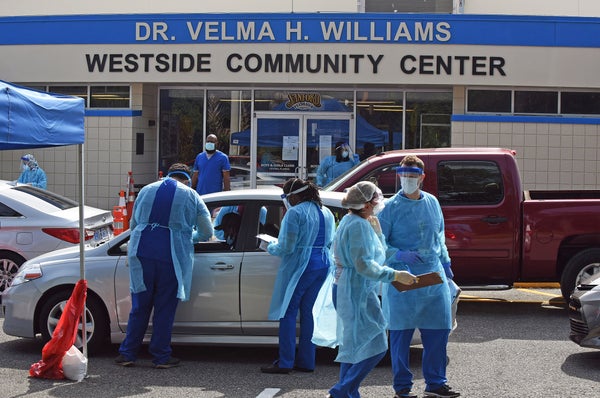
For example, in Louisiana—one of the first states to report data by race and ethnic group—testing teams went to poorer neighbourhoods to reach people without cars, who would have trouble making it to drive-through testing sites. Similarly, in May, New York announced a programme designed specifically to reach communities of colour.
Outreach must extend beyond testing to all aspects of the response, says Evelynn Hammonds, a historian of medicine at Harvard University in Cambridge, Massachusetts. Clinical trials, for example, must actively work to recruit a diverse population, otherwise the treatments and vaccines might not be equally effective. “We already know there’s a real problem with making sure that populations that are enlisted into clinical trials need to be diverse,” Hammonds says.
Communities of colour have historically been mistrustful of health systems, in part because they have been underserved or exploited. So, researchers must build relationships with these communities so that trials for COVID-19 treatments and vaccinations include people from all ethnic and racial groups, Hammonds says.
And hospitals in neighbourhoods that are likely to see a surge in cases because they serve more severely affected groups should be equipped sufficiently and in advance with protective equipment and ventilators, says Jones, who was president of the American Public Health Association in 2016. She calls for a plan to direct comparatively more resources into neighbourhoods where there are known to be higher incidences of chronic conditions. “If we know that these neighbourhoods are the ones being adversely impacted, then we need to move the ventilators and the health staff there,” Jones says.
A coherent voice
Health agencies and legislators around the world are beginning to grapple with the challenge. As of early May, most state departments and counties in the United States had begun to report race and ethnicity alongside infection and death rates. The UK government is putting out similar calls for data transparency, and it announced in mid-April that it would launch an inquiry into the reasons why the disparities exist.
Billions of federal dollars in the United States have been deployed towards tackling the pandemic, but because emergencies such as this one require a coordinated response across national agencies, some have argued for a central commission that will represent the needs of minority racial and ethnic groups.
“The call is for a national coherent voice that starts to talk about these issues,” says Laurencin, who suggested such a commission in an editorial last month.
Hammonds says that such a group could be effective because local US leaders typically prescribe public-health guidance and decisions, and so far have differed in their response to the pandemic. She compared New York’s rapid yet measured response with that in Georgia, whose governor announced a gradual re-opening of the economy in mid-April—despite contrary advice from public-health experts. This pandemic could be an opportunity to deploy consistent attention towards the needs of underserved communities, she says. “If there is a positive to come out of this, that would be one of them.”
This article is reproduced with permission and was first published on May 18 2020.
Read more about the coronavirus outbreak from Scientific American here. And read coverage from our international network of magazines here.